ABSTRACT
The conventional stethoscope, though a clinical mainstay, is limited by subjectivity. Digital stethoscopes integrated with Artificial Intelligence (AI) offer a transformative solution, converting acoustic signals into objective electronic data for automated classification and predictive analytics. This review synthesizes evidence demonstrating that AI-enhanced auscultation significantly boosts diagnostic accuracy and scalability. Studies highlight improved classification of pediatric heart murmurs (AUC up to 0.92), reliable detection of valvular heart disease (e.g., 93.2% sensitivity for aortic stenosis), and identification of lung pathology (wheezes, crackles, pneumonia). Furthermore, these devices proved valuable in screening for left ventricular dysfunction and facilitating triage during the COVID-19 pandemic. Future integration of multimodal sensing (ECG), wearable sensors, and Internet-of-Medical-Things (IoMT) will enable continuous, personalized monitoring. Successful implementation hinges on regulatory oversight and standardization across diverse populations. AI-powered digital stethoscopes are poised to democratize access and advance precision medicine globally.
Keywords: Digital Stethoscope; Artificial Intelligence; Machine Learning; Auscultation; Heart Murmur; Diagnostic Accuracy; Telemedicine; Precision Medicine
INTRODUCTION
Since its invention in 1816, the stethoscope has remained an enduring symbol of clinical practice and a cornerstone of bedside diagnosis. Conventional auscultation, however, is inherently dependent on clinician skill, auditory acuity, and experience, introducing subjectivity that can result in misclassification of heart murmurs, delayed recognition of pulmonary pathology, and missed early signs of cardiovascular compromise [1]. Digital stethoscopes have emerged as a technological evolution, converting acoustic signals into electronic data that can be amplified, filtered, and visualized. When coupled with artificial intelligence (AI), these devices enable automated sound classification, predictive analytics, and continuous monitoring. AI algorithms have the capacity to detect subtle acoustic patterns beyond human perception, offering objective assessments that may enhance diagnostic accuracy and improve patient outcomes [2]. Evidence increasingly supports the clinical utility of AI-enhanced digital stethoscopes. Multiple studies have demonstrated improved detection of pediatric heart murmurs, neonatal respiratory distress, valvular heart disease, and chronic pulmonary conditions. Furthermore, these devices provide cost-effective, non-invasive solutions suitable for telemedicine and resource-limited settings [3].
This review synthesizes current clinical evidence, technological innovations, and future directions for AI-integrated digital stethoscopes.
MATERIALS AND METHODS
A literature review was conducted using PubMed, Scopus, and Web of Science for publications from 2010 to 2025. Search terms included “digital stethoscope,” “artificial intelligence,” “machine learning,” “heart murmur,” and “respiratory auscultation,” with reference lists of relevant articles screened for additional studies. Eligible studies included prospective, comparative, and randomized clinical trials evaluating digital stethoscopes, with or without AI integration. Studies were included if they focused on cardiology, pulmonology, or pediatric populations, and reported objective diagnostic outcomes, including sensitivity, specificity, accuracy, or area under the receiver operating characteristic curve (AUC). Data extracted comprised study population characteristics, technological specifications, clinical focus, and diagnostic performance. Two independent reviewers performed data extraction, with discrepancies resolved by consensus. Findings were synthesized narratively and presented in tabular form, highlighting the comparative performance of AI-assisted versus conventional auscultation.
Clinical Utility and Evidence of AI-Enhanced Digital Stethoscopes
Digital stethoscopes convert mechanical vibrations into electronic signals using microphones or piezoelectric sensors, which can be amplified, filtered, and visualized in real time. Integration with artificial intelligence (AI) enhances their functionality, enabling automated classification of heart and lung sounds, predictive modeling, and longitudinal monitoring [4]. Signal processing techniques reduce noise and improve waveform fidelity, while deep learning algorithms, including convolutional neural networks (CNNs) and long short-term memory (LSTM) networks, support multi-class sound classification and early detection of physiological abnormalities. Connectivity with mobile devices, cloud platforms, and electronic health records facilitates telemedicine, remote consultation, and continuous patient monitoring. By transforming auscultation from a subjective skill into an objective and reproducible diagnostic process, AI-powered digital stethoscopes are particularly advantageous in populations where subtle physiological variations are clinically significant, such as neonates, pediatric patients, and critically ill adults.
Clinical evidence supports their utility across cardiology, pediatrics, and pulmonology. In children, heart murmurs are common and often benign, yet traditional auscultation is prone to misclassification. Zhou et al. [5] demonstrated that deep learning applied to digital stethoscope recordings achieved AUC values of 0.92, 0.83, and 0.88 for normal heart sounds, innocent murmurs, and pathological murmurs, respectively, enabling objective assessment and early intervention. For pediatric respiratory conditions, digital auscultation improved detection of wheezes, crackles, and stridor relative to conventional methods; Kevat et al. [6] reported higher sensitivity for wheezes and 100% concordance for crackles, while the PERCH study [7] confirmed reliable identification of abnormal lung sounds in children with pneumonia in low-resource settings. In neonates, AI-assisted digital stethoscopes facilitated early recognition of respiratory distress, with Grooby et al. [8] reporting 85% specificity and 66.7% sensitivity. In adult cardiology, AI-enhanced auscultation improved detection of valvular heart disease, with Chorba et al. [9] achieving 76.3% sensitivity and 91.4% specificity for murmurs, reaching 93.2% sensitivity for moderate-to-severe aortic stenosis and 94.6% specificity for mitral regurgitation. AI-guided screening in peripartum women nearly doubled detection of left ventricular systolic dysfunction compared with conventional assessment (4.1% vs. 2.0%) in a trial by Adedinsewo et al. [10], while integration with single-lead ECGs further enhanced early detection of asymptomatic left ventricular dysfunction (AUC 0.85; sensitivity 77.5%; specificity 78.3%) [11]. In pulmonology, AI-assisted auscultation improved diagnosis and monitoring of chronic respiratory diseases, including interstitial lung disease and chronic obstructive pulmonary disease, with deep learning models achieving AUC >80% when combined with lung imaging [12]. During the COVID-19 pandemic, digital stethoscopes facilitated rapid triage and severity prediction based on lung sounds, enhancing patient management in resource-limited and telemedicine settings [13]. Collectively, these findings demonstrate that AI-integrated digital stethoscopes provide objective, reproducible, and scalable assessments, enhancing early detection, clinical decision-making, and accessibility across diverse patient populations.
Discussion and Meta-Analysis of AI-Enhanced Digital Stethoscope Studies
Across pediatric, cardiac, and pulmonary populations, AI-assisted digital stethoscopes consistently enhance diagnostic accuracy, objectivity, and early detection. In pediatrics, these devices improve heart murmur classification [5], respiratory sound detection [5,6], and pneumonia identification in low-resource settings [7], while supporting timely intervention for neonatal respiratory distress [8]. In adult cardiology, AI-guided auscultation enables reliable detection of valvular heart disease [9], peripartum cardiomyopathy [10], and asymptomatic left ventricular systolic dysfunction [11], providing scalable, non-invasive screening that can reduce reliance on echocardiography. In pulmonology, deep learning applied to lung sounds, alone or combined with imaging modalities, achieves high accuracy for chronic respiratory diseases such as interstitial lung disease and chronic obstructive pulmonary disease (Table 1) [12], and facilitates rapid assessment of infectious conditions including COVID-19 [13]. Collectively, AI-powered digital auscultation decreases inter-observer variability, standardizes measurements, and supports timely clinical decision-making, offering particular advantages in pediatric populations and resource-limited environments.
|
Condition / Focus |
Technology Used |
Outcome Metrics |
Key Findings |
Study |
|
Pediatric heart murmurs |
Deep learning algorithm + digital stethoscope |
AUC: Normal 0.92, Innocent Murmurs 0.83, Pathologic 0.88 |
Multi-class classification of pediatric heart sounds (normal, innocent murmurs, pathologic murmurs) |
Zhou et al., 2024 |
|
Pediatric respiratory conditions |
Digital stethoscope |
Sensitivity: 100% for crackle detection; improved wheeze detection |
Higher sensitivity than clinician auscultation in detecting wheezes; 100% concordance for crackle detection |
Kevat et al., 2017 |
|
Pediatric respiratory sounds |
Digital stethoscope |
Sensitivity for wheeze: higher than traditional auscultation |
Enhanced detection of wheezes, crackles, and stridor vs traditional auscultation |
Zhou et al., 2024 |
|
Pediatric pneumonia diagnosis |
Digital stethoscope |
Diagnostic value in low-resource settings; more prevalent in severe cases |
Captured crackles and wheezes; higher prevalence in severe pneumonia |
PERCH Study, 2019 |
|
Neonatal respiratory distress |
Digital stethoscope + RUSBoost classifier |
Specificity: 85%; Sensitivity: 66.7%; Accuracy: 81.8% |
Early prediction of respiratory distress in term newborns |
Grooby et al., 2022 |
|
Cardiac murmurs and valvular disease |
Deep learning + digital stethoscope |
Sensitivity: 93.2% (Aortic Stenosis); Specificity: 94.6% (Mitral Regurgitation) |
High sensitivity and specificity for detecting murmurs, moderate-to-severe aortic stenosis, and mitral regurgitation |
Chorba et al., 2021 |
|
Peripartum cardiomyopathy |
AI-guided digital stethoscope |
Detection rate: 4.1% AI group; 2.0% control group |
Improved detection of LVSD in peripartum women, doubling detection rates |
Adedinsewo et al., 2024 |
|
Left ventricular systolic dysfunction |
Digital stethoscope + ECG |
AUC: 0.85; Sensitivity: 77.5%; Specificity: 78.3% |
Early detection of asymptomatic LVSD using CNN model |
Guo et al., 2025 |
|
Pulmonary diseases (ILD, COPD, COVID-19) |
Deep learning + digital stethoscope |
AUC: >80% for chronic lung diseases |
AI-assisted analysis of lung sounds for diagnosis and prognosis |
Glangetas et al., 2021 |
|
Chronic lung conditions (ILD, COPD) |
Deep learning + digital stethoscope |
AUC: >80% in diagnosing ILD and COPD |
Digital stethoscopes with AI models offer an alternative to traditional diagnostic techniques |
Siebert et al., 2023 |
|
COVID-19 diagnosis and prognosis |
AI-powered digital stethoscope |
Fast and consistent diagnoses; beneficial for telemedicine |
AI-driven analysis enabled rapid, consistent diagnosis and severity assessment |
Glangetas et al., 2021 |
Table 1: Recent Studies on Digital Stethoscopes in Cardiology, Pulmonology, and Pediatrics
AI-enhanced stethoscopes represent a paradigm shift, transforming a traditionally subjective skill into an objective diagnostic process. Evidence-based studies confirm their superiority for detecting pediatric murmurs, neonatal respiratory distress, valvular heart disease, and chronic pulmonary conditions (Table 2), with benefits including improved diagnostic accuracy, earlier interventions, reduced healthcare costs, and increased access in low-resource and telemedicine contexts. Nevertheless, challenges persist: clinician training, integration into clinical workflows, and standardization of AI models across diverse populations remain essential. Trust in algorithmic outputs, regulatory approval, and ongoing performance validation across age groups, comorbidities, and ethnicities are critical for safe implementation. Data privacy, security, and interoperability must also be addressed, particularly in telehealth and Internet-of-Medical-Things (IoMT)–enabled systems [3].
|
Population / Condition |
AI Performance |
Clinical Interpretation |
Significance for Practice |
Study |
|
Pediatric Heart Murmur |
AUC 0.92 / 0.83 / 0.88 |
Accurate classification; reduces misdiagnosis |
Supports early detection, standardized evaluation, clinician confidence |
Zhou et al., 2024 |
|
Pediatric Respiratory Sounds |
High sensitivity; crackle 100% concordance |
Objective detection of wheezes, crackles, stridor |
Early intervention, reduces subjective variability |
Kevat et al., 2017 & Zhou et al., 2024 |
|
Pediatric Pneumonia |
>1,000 lung recordings; abnormal sounds prevalent |
Identifies severe pneumonia |
Cost-effective, non-invasive diagnosis in low-resource settings |
PERCH Study, 2017 |
|
Neonatal Respiratory Distress |
RUSBoost: 85% specificity, 66.7% sensitivity, 81.8% accuracy |
Detects early respiratory compromise |
Enables timely NICU intervention |
Grooby et al., 2022 |
|
Valvular Heart Disease |
Sensitivity 76.3%, specificity 91.4%; aortic stenosis 93.2%, mitral regurgitation 94.6% |
Accurate murmur and valve detection |
Non-invasive screening, reduces echocardiography dependence |
Chorba et al., 2021 |
|
Peripartum Cardiomyopathy |
AI doubled LVSD detection (4.1% vs 2.0%) |
Early identification in obstetric population |
Facilitates timely management where echo is limited |
Adedinsewo et al., 2025 |
|
Asymptomatic LVSD |
AUC 0.85, sensitivity 77.5%, specificity 78.3% |
Detects subclinical LV dysfunction |
Scalable, non-invasive screening for early intervention |
Guo et al., 2024 |
Table 2: Clinical Interpretation and Significance of evidence-based clinical studies in the era of artificial intelligence digital stethoscope
The COVID-19 pandemic further highlighted the utility of AI-integrated digital stethoscopes in decentralized care. Algorithms facilitated rapid triage and disease severity assessment, underscoring their potential in telehealth, pandemic preparedness, and low-resource settings. As clinical datasets expand, AI models are expected to become increasingly sophisticated, potentially integrating multimodal signals such as electrocardiography, pulse oximetry, and respiratory rate—to deliver holistic, patient-specific diagnostic outputs. These advances position AI-enhanced auscultation as a cornerstone of precision, accessible, and data-driven healthcare.
Future Technological Perspectives, Limitations, and Directions
Emerging digital stethoscope technologies are set to transform auscultation through continuous, non-invasive, and context-aware monitoring. Flexible and wearable devices, such as epidermal acoustic sensors and soft polymer piezoelectric systems, enable high-fidelity sound acquisition without tubing interference, improved chest conformity, and wireless transmission to mobile and cloud platforms, making them especially suitable for pediatric, neonatal, and long-term care applications [14,15]. Integration of heart and lung sound analysis with complementary signals including electrocardiography, pulse oximetry, respiratory rate sensors, and motion detectors permits multimodal diagnostics, allowing AI algorithms to detect compound pathologies, such as heart failure exacerbations, by analyzing synchronous physiologic data [16]. AI can also establish individualized acoustic baselines, improving sensitivity, reducing false positives, and supporting early intervention in chronic conditions such as heart failure and asthma [16]. Augmented reality and workflow integration enable clinicians to visualize auscultation data and AI-guided diagnostic suggestions in real time, enhancing efficiency, standardization, and documentation within electronic health records [17].
Future digital stethoscopes will increasingly leverage interoperability standards, including FHIR, HL7, DICOM-WAVE, and IEEE 11073, enabling secure data exchange, real-time streaming, and integration with telehealth platforms, hospital systems, and predictive analytics frameworks for population health management and AI-assisted triage [18]. Despite these advances, significant challenges remain. High-quality annotated datasets are essential for robust algorithm training, yet variability in recording environments, patient movement, and background noise may compromise model performance. Many studies remain single-center or region-specific, limiting generalizability and emphasizing the need for multicenter validation. Regulatory and ethical considerations—including compliance with medical device regulations, data privacy, and algorithm transparency—are critical to build clinician trust. Cost and accessibility may restrict deployment, particularly in low-income regions, and successful integration requires alignment with clinical workflows and acceptance by healthcare teams. Collaborative efforts among engineers, clinicians, data scientists, and policymakers are essential for safe, effective, and equitable implementation.
Looking forward, next-generation AI-integrated digital stethoscopes will combine wearable technologies, multimodal sensing, and advanced analytics to enable continuous monitoring, personalized diagnostics, and augmented clinical decision support. IoMT-enabled devices will facilitate remote consultations and longitudinal tracking of patient-specific acoustic profiles, enhancing early detection of pathophysiological changes. Multi-modal fusion of heart and lung sounds with ECG, pulse oximetry, respiratory rate, and motion data will allow comprehensive cardiopulmonary assessment, while predictive AI algorithms may forecast disease progression, hospital readmissions, and acute exacerbations, guiding proactive interventions. These innovations promise to improve diagnostic precision, democratize access to care, and transform patient management across diverse clinical settings (Figure 1) [3].
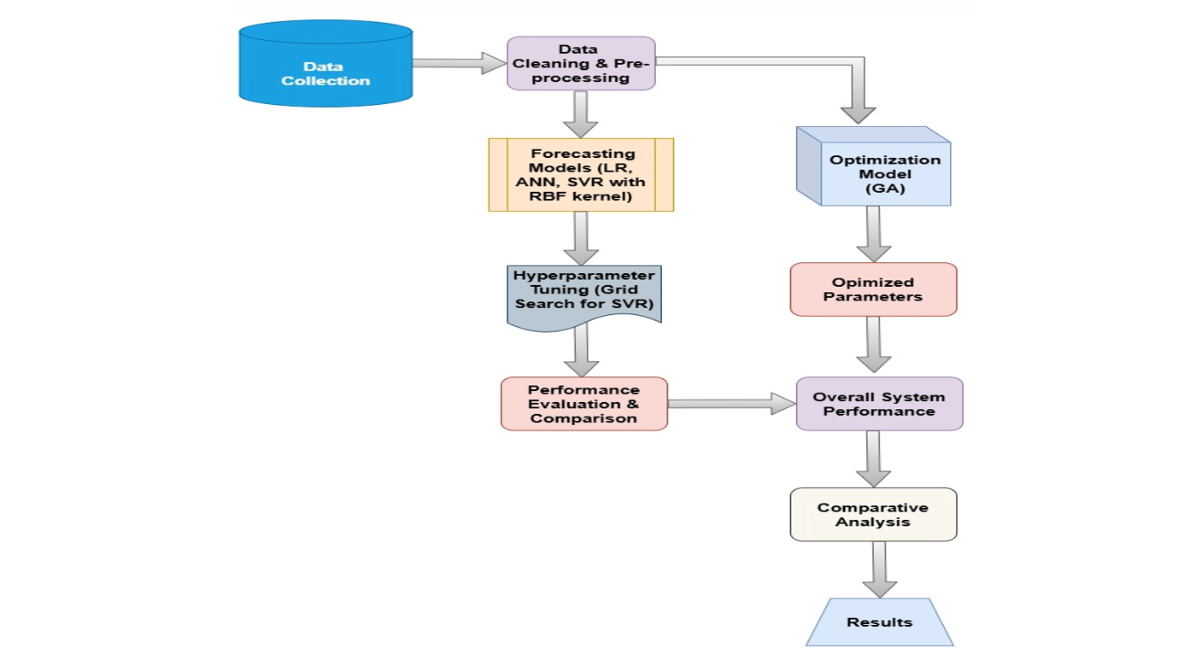
Figure 1: AI-Integrated Digital Stethoscope: Transforming Auscultation into Precision Diagnostics.
Note: AI-Enhanced Digital Auscultation. This figure illustrates the evolution and application of digital stethoscopes integrated with Artificial Intelligence (AI), representing a paradigm shift toward precision medicine. The schematic is divided into three interconnected columns detailing the transformation from traditional methods to continuous, personalized diagnostics.
CONCLUSION
In conclusion, AI-enhanced digital stethoscopes represent a transformative evolution in evidence-based medicine. By improving diagnostic accuracy, reducing inter-observer variability, and enabling early detection of cardiac, pulmonary, and neonatal conditions, they offer substantial clinical benefits. Current evidence supports their utility in pediatric heart murmur classification, neonatal respiratory distress, peripartum cardiomyopathy, chronic pulmonary diseases, and COVID-19 management. Continued technological innovation including wearable devices, sensor fusion, personalized acoustic profiling, and telemedicine integration alongside robust datasets, regulatory oversight, and clinician training, will be crucial for widespread adoption. As these systems mature, AI-powered digital stethoscopes are poised to become indispensable tools for precision, patient-centered care, expanding access, and improving outcomes globally.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest directly related to the content of this manuscript. Professor E. Andrès has conducted fundamental and clinical research under institutional contracts with Alcatel-Lucent and the French National Technology Agency
REFERENCES
- Andrès E, Gass R, Brandt C. Etat de l’art sur les stéthoscopes électroniques en 2015. Médecine thérapeutique. 2015;21:319-2. [Google Scholar]
- Arjoune Y, Nguyen TN, Doroshow RW, Shekhar R. Technical characterisation of digital stethoscopes: towards scalable artificial intelligence-based auscultation. Journal of medical engineering & technology. 2023;47(3):165-78. [Crossref] [Google Scholar] [PubMed]
- Seah JJ, Zhao J, Wang DY, Lee HP. Review on the advancements of stethoscope types in chest auscultation. Diagnostics. 2023;13(9):1545. [Crossref] [Google Scholar] [PubMed]
- Kim Y, Hyon Y, Woo SD, Lee S, Lee SI, et al. Evolution of the stethoscope: advances with the adoption of machine learning and development of Wearable devices. Tuberculosis and respiratory diseases. 2023;86(4):251. [Crossref] [Google Scholar] [PubMed]
- Zhou G, Chien C, Chen J, Luan L, Chen Y, et al. Identifying pediatric heart murmurs and distinguishing innocent from pathologic using deep learning. Artificial Intelligence in Medicine. 2024;153:102867. [Crossref] [Google Scholar] [PubMed]
- Kevat AC, Kalirajah A, Roseby R. Digital stethoscopes compared to standard auscultation for detecting abnormal paediatric breath sounds. European Journal of Pediatrics. 2017;176(7):989-92. [Crossref] [Google Scholar] [PubMed]
- McCollum ED, Park DE, Watson NL, Buck WC, Bunthi C, et al. Listening panel agreement and characteristics of lung sounds digitally recorded from children aged 1–59 months enrolled in the Pneumonia Etiology Research for Child Health (PERCH) case–control study. BMJ open respiratory research. 2017;4(1). [Crossref] [Google Scholar] [PubMed]
- Grooby E, Sitaula C, Tan K, Zhou L, King A, et al. Prediction of neonatal respiratory distress in term babies at birth from digital stethoscope recorded chest sounds. In2022 44th Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC) 2022 (pp. 4996-4999). IEEE. [Crossref] [Google Scholar] [PubMed]
- Chorba JS, Shapiro AM, Le L, Maidens J, Prince J, et al. Deep learning algorithm for automated cardiac murmur detection via a digital stethoscope platform. Journal of the American Heart Association. 2021;10(9):e019905. [Crossref] [Google Scholar] [PubMed]
- Adedinsewo DA, Morales-Lara AC, Afolabi BB, Kushimo OA, Mbakwem AC, et al. Artificial intelligence guided screening for cardiomyopathies in an obstetric population: a pragmatic randomized clinical trial. Nature Medicine. 2024;30(10):2897-906. [Crossref] [Google Scholar] [PubMed]
- Guo L, Pressman GS, Kieu SN, Marrus SB, Mathew G, et al. Automated detection of reduced ejection fraction using an ECG-enabled digital stethoscope: a large cohort validation. JACC: Advances. 2025;4(3):101619. [Crossref] [Google Scholar] [PubMed]
- Siebert JN, Hartley MA, Courvoisier DS, Salamin M, Robotham L, et al. Deep learning diagnostic and severity-stratification for interstitial lung diseases and chronic obstructive pulmonary disease in digital lung auscultations and ultrasonography: clinical protocol for an observational case–control study. BMC pulmonary medicine. 2023;23(1):191. [Crossref] [Google Scholar] [PubMed]
- Glangetas A, Hartley MA, Cantais A, Courvoisier DS, Rivollet D, et al. Deep learning diagnostic and risk-stratification pattern detection for COVID-19 in digital lung auscultations: clinical protocol for a case–control and prospective cohort study. BMC pulmonary medicine. 2021;21(1):103. [Crossref] [Google Scholar] [PubMed]
- Lakhe A, Sodhi I, Warrier J, Sinha V. Development of digital stethoscope for telemedicine. Journal of medical engineering & technology. 2016;40(1):20-4. [Crossref] [Google Scholar] [PubMed]
- Yilmaz G, Rapin M, Pessoa D, Rocha BM, de Sousa AM, et al. A wearable stethoscope for long-term ambulatory respiratory health monitoring. Sensors. 2020;20(18):5124. [Crossref] [Google Scholar] [PubMed]
- Duggan D, Sarana V, Factor A, Shelevytska V, Temko A, et al. Towards a Wearable, High Precision, Multi-Functional Stethoscope. In2024 46th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC) 2024 (pp. 1-4). IEEE. [Crossref] [Google Scholar] [PubMed]
- Kono Y, Miura K, Kasai H, Ito S, Asahina M, et al. Breath measurement method for synchronized reproduction of biological tones in an augmented reality auscultation training system. Sensors. 2024;24(5):1626. [Crossref] [Google Scholar] [PubMed]
- Das A, Adams K, Stoicoiu S, Kunhiabdullah S, Mathew A. Amplification of Heart Sounds Using Digital Stethoscope in Simulation-Based Neonatal Resuscitation. American Journal of Perinatology. 2024;41(S 01):e2485-8. [Crossref] [Google Scholar] [PubMed]
Article Processing Timeline
| 2-5 Days | Initial Quality & Plagiarism Check |
| 15 Days |
Peer Review Feedback |
| 85% | Acceptance Rate (after peer review) |
| 30-45 Days | Total article processing time |
Indexed In
ResearchBib
Sindexs
OAJI
DOAJ
CrossRef
PubMed
MEDLINE
EBSCO A-Z / Host
OCLC - WorldCat
Journal Flyer