ABSTRACT
Severely calcified coronary artery disease poses a substantial technical challenge during Percutaneous Coronary Intervention (PCI), particularly in patients deemed ineligible for surgical revascularization due to multiple comorbidities. We present the case of a 58-year-old male with end-stage renal disease, liver cirrhosis, prior myocardial infarction with in-stent restenosis, and triple-vessel disease involving the left main and bifurcation branches. The patient was refused for CABG by multiple centers and presented with unstable angina. Conventional balloon dilation failed due to severe calcification, and the procedure was aborted due to high perforation risk. Intra Vascular Lithotripsy (IVL) was then employed to safely modify the calcified lesions, enabling successful bifurcation stenting using the double-kissing crush technique. The patient was discharged in stable condition, with complete symptom resolution. This case highlights IVL as a critical and effective tool for lesion preparation in patients with complex calcified anatomy, especially when traditional options are limited or unsafe.
Keywords: Intravascular Lithotripsy; Calcified Coronary Disease; PCI; In-Stent Restenosis; Left Main Bifurcation; CABG-Ineligible; High-Risk Intervention; Case Report
INTRODUCTION
Severe coronary artery calcification represents a significant challenge during Percutaneous Coronary Intervention (PCI), frequently acting as a formidable barrier to optimal vessel dilation and stent deployment [1]. The presence of calcific stenosis not only complicates device delivery but is also strongly associated with an increased risk of coronary artery perforation, which occurs in approximately 0.5% to 1.0% of PCI procedures involving calcified lesions. In contrast, coronary perforation rates in non-calcified vessels are substantially lower, typically less than 0.2% [2]. Importantly, coronary perforation significantly worsens clinical outcomes, being linked to a 13-fold increase in in-hospital Major Adverse Cardiovascular Events (MACE) and a fivefold increase in 30-day mortality [3]. This underscores the critical need for precise procedural decision-making during PCI, especially in complex anatomical scenarios such as Left Main (LM) coronary artery disease and bifurcation lesions, where the stakes are higher due to the large myocardial territory at risk [4].
The management of heavily calcified lesions becomes even more challenging when surgical revascularization via Coronary Artery Bypass Grafting (CABG) is contraindicated due to patient comorbidities or other high-risk factors. In such contexts, alternative percutaneous strategies that safely modify calcified plaques are essential. While Rotational Atherectomy (RA) has been a traditional tool for calcified lesions, it carries inherent risks of complications such as perforation, dissection, and the "no-reflow" phenomenon, particularly in complex anatomies like bifurcations or In-Stent Restenosis (ISR).
Intra Vascular Lithotripsy (IVL) has emerged as a novel and promising technique designed specifically to address the problem of severe coronary calcification. IVL utilizes controlled acoustic shockwaves to fracture both superficial and deep calcium deposits, thereby increasing vessel compliance and facilitating optimal stent expansion [5]. Meta-analyses and multicenter registries report procedural success rates—defined as residual stenosis of less than 50% with successful stent deployment—of approximately 95%. Moreover, clinical and angiographic success rates consistently range between 97% and 98%, highlighting the safety and efficacy profile of IVL in real-world practice [6].
In the current report, we present a complex clinical scenario where IVL served as a crucial, life-saving intervention. Our patient exhibited severe multivessel coronary calcification with in-stent restenosis and was deemed ineligible for CABG due to multiple serious comorbidities. This case exemplifies the expanding role of IVL as an effective tool in the interventional cardiologist’s armamentarium, particularly in high-risk patients with limited revascularization options.
CASE PRESENTATION
A 58-year-old male with a complex medical background presented with recurrent episodes of unstable angina. His comorbidities included: liver cirrhosis secondary to cured hepatitis C, End-Stage Renal Disease (ESRD) requiring hemodialysis five times per week, type 2 diabetes mellitus, a history of anterior myocardial infarction with prior LAD stenting five years earlier, and underlying myopathy.
The patient had been evaluated at multiple tertiary centers, all of which declined surgical intervention due to his high-risk status and multiple comorbidities. At presentation to Al-Bashir Hospital, he experienced ongoing chest pain consistent with unstable angina. Coronary angiography revealed: 60% calcified stenosis in the Left Main (LM) artery, 70% calcified stenosis at the ostium of the Circumflex (Cx), and In-Stent Restenosis (ISR) in the previously stented LAD segment with significant calcification adjacent to the under expanded stent (Figure 1).
Laboratory and Imaging Findings revealed: Serum Creatinine: 492 µmol/L (markedly elevated), Urea: 11.1 mmol/L (elevated), high-sensitivity Troponin: 3094.7 ng/L (elevated), INR: 2.17, and echocardiogram showed preserved left ventricular ejection fraction (EF = 55%) with mild-to-moderate mitral regurgitation (MR grade 1–2).
Given the urgent clinical picture and rejection of CABG by multiple centers, a percutaneous coronary intervention (PCI) approach was pursued. The procedure was initiated with the insertion of a 2.0 × 5 mm semi-compliant balloon into the LAD. However, this revealed a bulging calcified plaque between the collapsed stent and the arterial wall, indicating a high risk of arterial perforation. The procedure was temporarily halted due to safety concerns (Figure 2).
In the absence of other viable options, intravascular lithotripsy (IVL) was employed—a challenging and resource-intensive choice, particularly in a low-income setting such as Jordan. Shockwave Lithotripsy was applied with 70 pulses to the LAD and 10 pulses to the Cx. This allowed successful modification of the calcified lesions, creating a safe environment for definitive bifurcation intervention. A Double-Kiss Crush (DK-Crush) stenting technique was then performed for the LM-LAD-Cx bifurcation, employing a 1:1:1 Medina classification strategy (Figure 3). A new drug-eluting stent was deployed in the LAD, with final angiography showing fully patent three-vessel flow (Figure 4).
The patient remained hemodynamically stable and was discharged on day 2 post-procedure in good clinical condition. He was maintained on dual antiplatelet therapy (DAPT) and reported complete resolution of anginal symptoms. Discharge medications included dual antiplatelet therapy (DAPT with Aspirin and Clopidogrel), a high-intensity statin, and his routine medications for other comorbidities. A follow-up echocardiogram at one month showed stable cardiac function, and the patient reported complete and sustained resolution of anginal symptoms
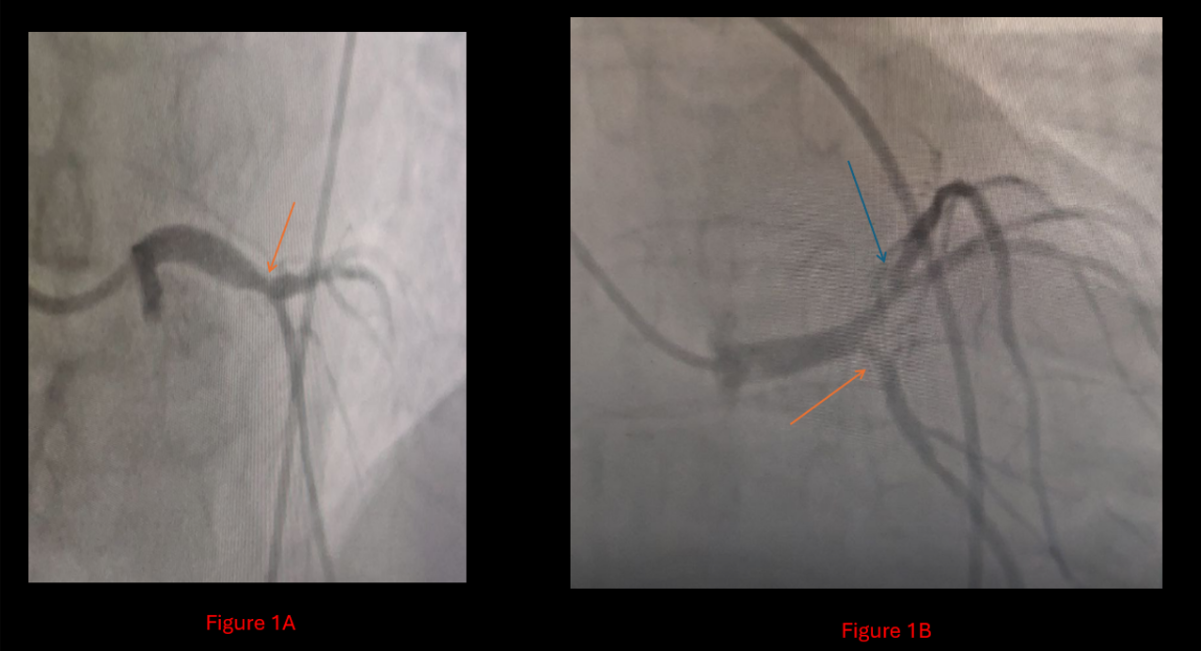
Figure 1A: Diagnostic catheterization showing 60% left main artery stenosis, and for
Figure 1B: A 70% ostial circumflex stenosis is indicated by the orange arrow, in addition to In-Stent Restenosis (ISR) in the left anterior descending artery with significant calcification between the collapsed stent and the arterial wall is indicated by the blue arrow
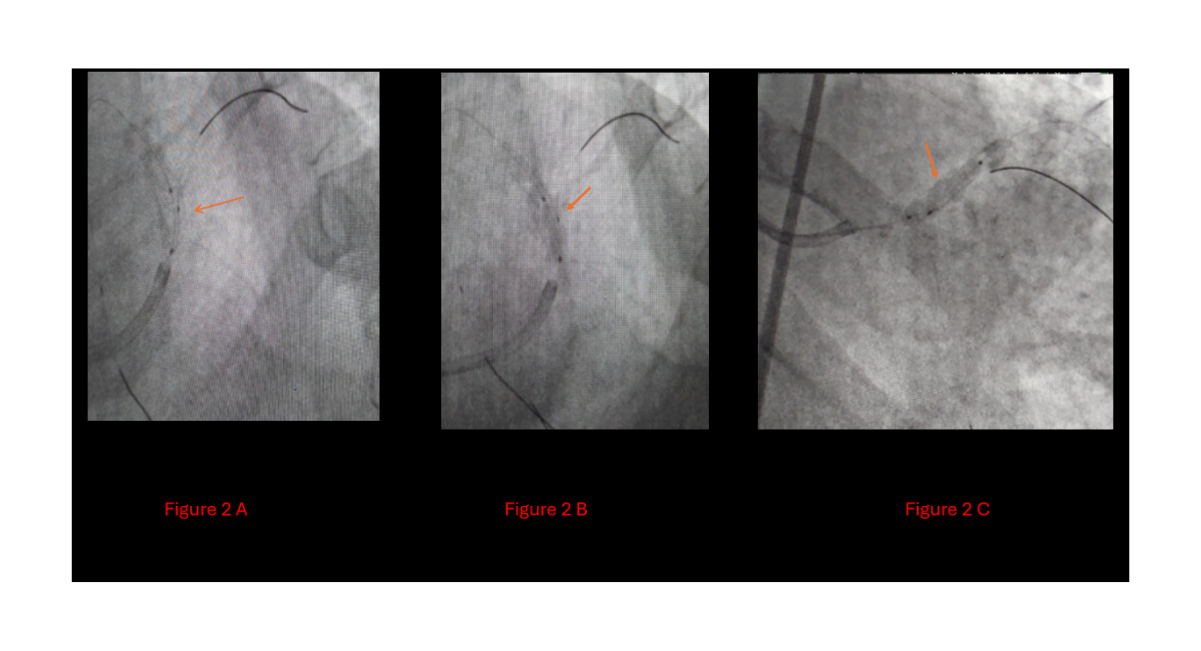
Figure 2A: A semicompliant 2*5 balloon was inserted for balloon stent dilatation,
2B: Calcium-deposited bulge,
2C: Indicating a high risk of perforation with the ongoing procedure
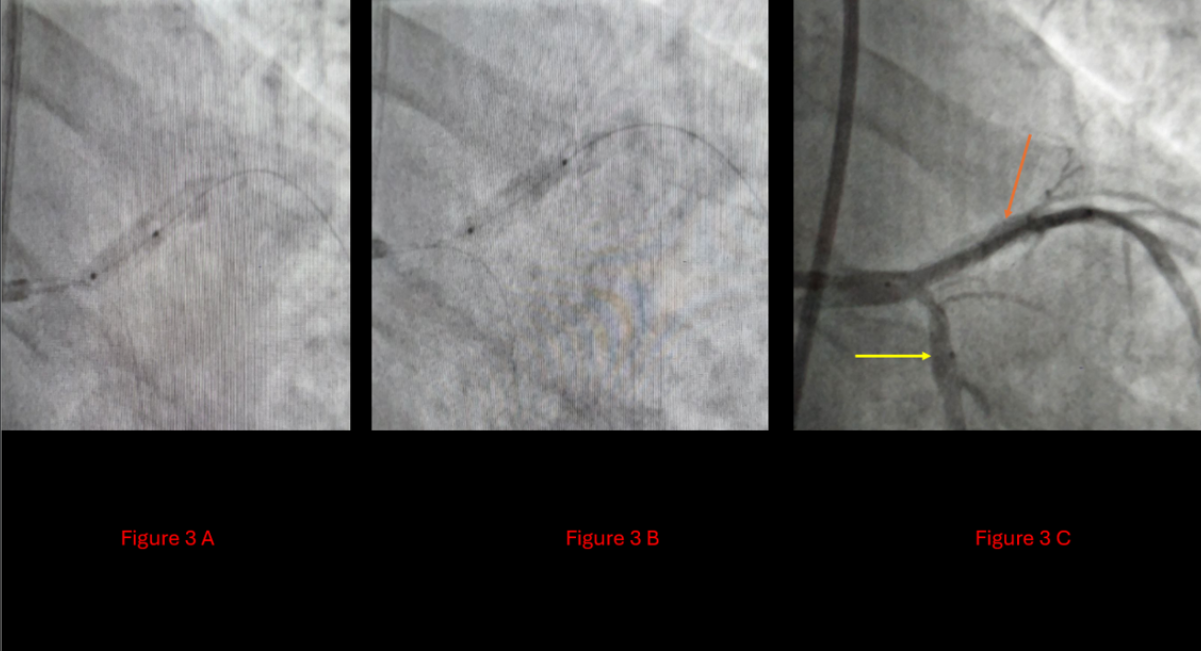
Figure 3A: Insertion of the shockwave balloon
3B: Postshock wave non-compliant balloon
3C: Orange arrow: LAD post shockwave, Yellow arrow: Cx post shockwave

Figure 4: Showing the outcome after the DKC technique.
4A: Orange arrow: new stent in the LAD, yellow arrow: stent in the Cx.
4B: Patent LM, LAD, and cx
DISCUSSION
Patient Complexity
The success of this complex intervention was contingent upon both the advanced technical equipment available and the professional experience of the heart team. This case involves a 58-year-old male with multiple significant comorbidities, including liver cirrhosis, end-stage renal disease, a history of MI, DM, and myopathies, posing a formidable challenge in cardiovascular intervention. The case demanded meticulous evaluation and expert clinical judgment, especially in the absence of guideline-based solutions. Thorough anatomical assessment via coronary angiography revealed severe left main bifurcation calcification and in-stent restenosis (ISR). Coronary artery bypass grafting (CABG) was contraindicated due to the patient's high surgical risk. Repeated balloon dilatation was avoided due to the substantial risk of coronary perforation in calcified segments, and rational use of rotational atherectomy or other debulking devices was limited by ISR and patient frailty.
While intravascular imaging (IVUS or OCT) is typically recommended to optimize lesion assessment and procedural planning, financial limitations prevented its application. Despite this, diagnostic angiography provided sufficient insight to proceed with a high-stakes yet targeted interventional strategy
Reaching the Solution
Intravascular lithotripsy (IVL) is an emerging modality for the treatment of severe coronary artery calcification. By delivering pulsatile sonic pressure waves, IVL fractures both superficial and deep calcium, improving vessel compliance while minimizing trauma to surrounding tissues. In this case, IVL was uniquely suited to disrupt the calcium burden, facilitate stent expansion, and allow safe revascularization using the Double Kissing Crush (DKC) technique for bifurcation disease. It represented the only feasible and safe solution, effectively modifying the calcified plaque and enabling the successful deployment of new stents.
Procedural Outcome
The outcome was exemplary. IVL performed as a single, definitive intervention—successfully modifying a heavily calcified bifurcation segment and resolving ISR with no complications. The ability to crush the previously underexpanded stent and deploy a new stent construct using a 1:1:1 DKC technique led to full luminal gain and angiographic success. This real-world application of IVL reinforces its growing role in complex, high-risk PCI settings.
Comparison with the Literature
This case parallels previous reports demonstrating IVL’s utility in similar scenarios—particularly ISR, left main stem disease, and eccentric calcification [7, 8]. The unique contribution of our case is its demonstration of IVL's application in a resource-limited environment for a patient with a confluence of high-risk features: surgical ineligibility, multivessel disease with ISR, and a critical complication during initial PCI. Meta-analyses have shown high procedural success (~95%) and minimal complication rates, echoing our experience. However, the unique combination of ISR, complex bifurcation disease, surgical ineligibility, and financial constraint highlights the innovation and decision-making required. Few reports capture this exact constellation, making this case a valuable addition to the literature
Procedural Outcome and Limitations
The procedural outcome was exemplary, achieved through meticulous planning and the strategic application of IVL. However, we must acknowledge the limitations inherent in this case. The absence of intravascular imaging meant we could not objectively quantify the calcium burden pre- or post-IVL or confirm the mechanism of stent expansion. Furthermore, the long-term outcomes in such complex patients remain to be fully characterized, though the patient's symptomatic relief at one month is highly encouraging.
Teaching Points
This case offers several critical teaching points for interventional cardiologists:
IVL as a Strategic Tool: IVL should be recognized as a primary option for lesion preparation in severely calcified coronaries, especially in patients who are poor surgical candidates.
Safety in Complex Anatomy: IVL can safely facilitate stent expansion in high-risk locations like the left main bifurcation and in areas of ISR, where atherectomy may be riskier.
Bail-Out Utility: This case demonstrates the life-saving potential of IVL as a bail-out strategy when conventional balloon techniques fail or are deemed too dangerous.
Heart Team Imperative: A collaborative heart team approach is essential for tailoring revascularization strategies in complex clinical and anatomical scenarios, even when surgery is not an option.
Resource-Aware Decision Making: In settings where intravascular imaging is unavailable, a thorough angiographic assessment and knowledge of advanced tools like IVL can still lead to successful outcomes.
CONCLUSION
This case highlights the pivotal role of Intravascular Lithotripsy (IVL) as a life-saving, frontline technique in managing severely calcified coronary lesions—especially in patients who are not surgical candidates due to significant comorbidities. IVL effectively addressed in-stent restenosis in the left main bifurcation, achieving stent expansion and procedural success without major complications. The case exemplifies how contemporary interventional tools, paired with individualized clinical judgment, can overcome guideline-limited scenarios. Ultimately, IVL emerges not just as a tool of convenience but as a transformative strategy in the treatment of complex coronary disease, particularly when traditional options fall short.
REFERENCES
- Giannini F, Candilio L, Mitomo S, Ruparelia N, Chieffo A, et, al. A practical approach to the management of complications during percutaneous coronary intervention. JACC Cardiovasc Interv. 2018 ;11(18):1797-810. [ Crossref] [ Google Scholar] [ PubMed]
- Saito Y, Kobayashi Y, Fujii K, Sonoda S, Tsujita K, et, al. CVIT 2023 clinical expert consensus document on intravascular ultrasound. Cardiovasc. Intervention Ther.. 2024;39(1):14. [ Google Scholar]
- Kinnaird T, Kwok CS, Kontopantelis E, Ossei-Gerning N, Ludman P, et, al. Incidence, determinants, and outcomes of coronary perforation during percutaneous coronary intervention in the United Kingdom between 2006 and 2013: An analysis of 527 121 cases from the British Cardiovascular Intervention Society Database. Circulation: Circ Cardiovasc Interv. 2016;9(8):e003449. [ Crossref] [ Google Scholar] [ PubMed]
- Members WC, Lawton JS, Tamis-Holland JE, Bangalore S, Bates ER, et, al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: Executive summary: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79(2):197-215 [ Crossref] [ Google Scholar] [ PubMed]
- Liang B, Gu N. Evaluation of the safety and efficacy of coronary intravascular lithotripsy for treatment of severely calcified coronary stenoses: Evidence from the serial disrupt CAD trials. Front. cardiovasc. med. 2021;8:724481. [ Crossref] [ Google Scholar] [ PubMed]
- Mhanna M, Beran A, Nazir S, Sajdeya O, Srour O, et,al. Efficacy and safety of intravascular lithotripsy in calcified coronary lesions: A systematic review and meta-analysis. Cardiovasc Revasc Med. 2022; 36:73-82. [ Crossref] [ Google Scholar] [ PubMed]
- Mahanta D, Deb P, Mohanan S, Acharya D, Das D, et, al. The Unique Role of Intravascular Lithotripsy (IVL) in Debulking the Nodular Calcium in Left Main Coronary Artery Bifurcation. Cureus. 2024;16(6). [ Crossref] [ Google Scholar] [ PubMed]
- Kassab K, Kassier A, Fischell TA. Intracoronary lithotripsy use for in-stent restenosis, including multilayer ISR. Cardiovasc Revasc Med. 2022;44:10-3. [ Crossref] [ Google Scholar] [ PubMed]
REFERENCES
Article Processing Timeline
| 2-5 Days | Initial Quality & Plagiarism Check |
| 15 Days |
Peer Review Feedback |
| 85% | Acceptance Rate (after peer review) |
| 30-45 Days | Total article processing time |
Journal Flyer