ABSTRACT
Background
Prosthetic Valve Thrombosis (PVT) is a life-threatening complication, particularly when involving left-sided mechanical valves. Coronary embolism secondary to PVT is exceedingly rare and poses a diagnostic and therapeutic challenge. Guidelines recommend urgent surgery, but options are limited in patients with unstable blood pressure or who are inoperable.
Case Summary
We present a rare case of a 50-year-old male with a history of double mechanical valve replacement on chronic warfarin therapy, who presented with symptoms of acute anterior STEMI. He was found to have a stuck aortic valve due to thrombus formation, with embolization into the left anterior descending artery (LAD) causing coronary obstruction. The patient was hemodynamically unstable (BP 90/60 mmHg) and had a subtherapeutic INR of 1.1. Surgery was deemed too high-risk. Full-dose tenecteplase was administered (⅓ intracoronary, ⅔ intravenous), followed by multiple aspiration catheter runs. The patient’s condition rapidly stabilized, with restoration of LAD patency and full valve mobility. No stents were used. Follow-up on day 3 showed complete thrombus resolution. He was discharged on day 4 on optimized anticoagulation.
Keywords: Prosthetic valve thrombosis, coronary embolism, stuck mechanical valve, tenecteplase, aspiration thrombectomy, off-label thrombolysis, valve-related STEMI.
INTRODUCTION
Mechanical prosthetic heart valves are widely used to treat advanced valvular heart disease; however, they carry lifelong risks, particularly related to thromboembolic events. A “stuck valve” refers to the mechanical obstruction of a prosthetic valve, most commonly caused by thrombus formation or fibrous pannus tissue, leading to restricted leaflet mobility and impaired cardiac function. Among those, thrombotic obstruction is the most common, accounting for up to 78% of cases, while pannus alone is responsible for about 10%, and a combination of both in another 10–12% [1].
The clinical consequences of a stuck valve can be severe, ranging from acute heart failure to cardiogenic shock. Mortality rates vary depending on the underlying cause and chosen intervention. Surgical intervention remains the gold standard for managing obstructive prosthetic valve thrombosis, particularly in hemodynamically stable patients. The most common surgical approach is redo valve replacement, where the thrombosed mechanical valve is removed and replaced with a new prosthetic valve. In selected cases, especially when the thrombus is localized and the valve structure is preserved, surgical thrombectomy or pannus resection may be considered. These procedures aim to restore normal leaflet motion without replacing the valve. However, in critically ill patients or those with contraindications to surgery, thrombolytic therapy may be a life-saving alternative. Despite being effective in some cases, surgical treatment still carries a high perioperative mortality—ranging from 15% to over 40% in unstable patients—highlighting the need for rapid diagnosis and individualized decision-making [2]. Surgical valve replacement remains the gold-standard treatment for obstructive prosthetic valve thrombosis (PVT), but in unstable or high-risk patients, mortality can exceed 40%. In contrast, thrombolytic therapy, although associated with bleeding risk, has demonstrated mortality rates of around 10–15% in selected populations and may be a viable alternative in emergencies [3].
The situation becomes even more complex when PVT is complicated by coronary artery embolism, a rare but catastrophic event that may result in acute ST-elevation myocardial infarction (STEMI). In such cases, timely diagnosis and individualized treatment are critical to improving outcomes. Despite its clinical relevance, there is a lack of structured data on patients who experience both prosthetic valve thrombosis and myocardial infarction.
This case highlights several clinical challenges, including the rare but life-threatening combination of prosthetic valve thrombosis and embolic myocardial infarction, hemodynamic instability limiting surgical options, and the absence of clear guidelines for dual-pathology management.
CASE PRESENTATION
Diagnosis
A 50-year-old male with a history of hypertension and double mechanical valve replacement five years ago, maintained on chronic warfarin therapy, presented to the emergency department with typical symptoms of acute myocardial infarction (MI). On arrival, he was hemodynamically unstable, with a blood pressure of 90/60 mmHg and a heart rate of 70 bpm. Routine MI workup, including ECG (Figure 1), revealed an isolated anterior ST-elevation MI (STEMI). Following standard guidelines, an echocardiogram was performed and demonstrated a severely elevated aortic valve gradient of 60 mmHg, suggestive of severe aortic stenosis (Figure 2). The INR was pending at that time. Urgent diagnostic coronary angiography via the radial approach was conducted. Fluoroscopy revealed a stuck mechanical aortic valve: one leaflet was completely immobile, while the other one was partially restricted. Additionally, a thrombus was visualized in the proximal part of the left anterior descending (LAD) artery. It was presumed that thrombus formation on the aortic valve had embolized during diastole into the LAD (Figure 3, video 1).
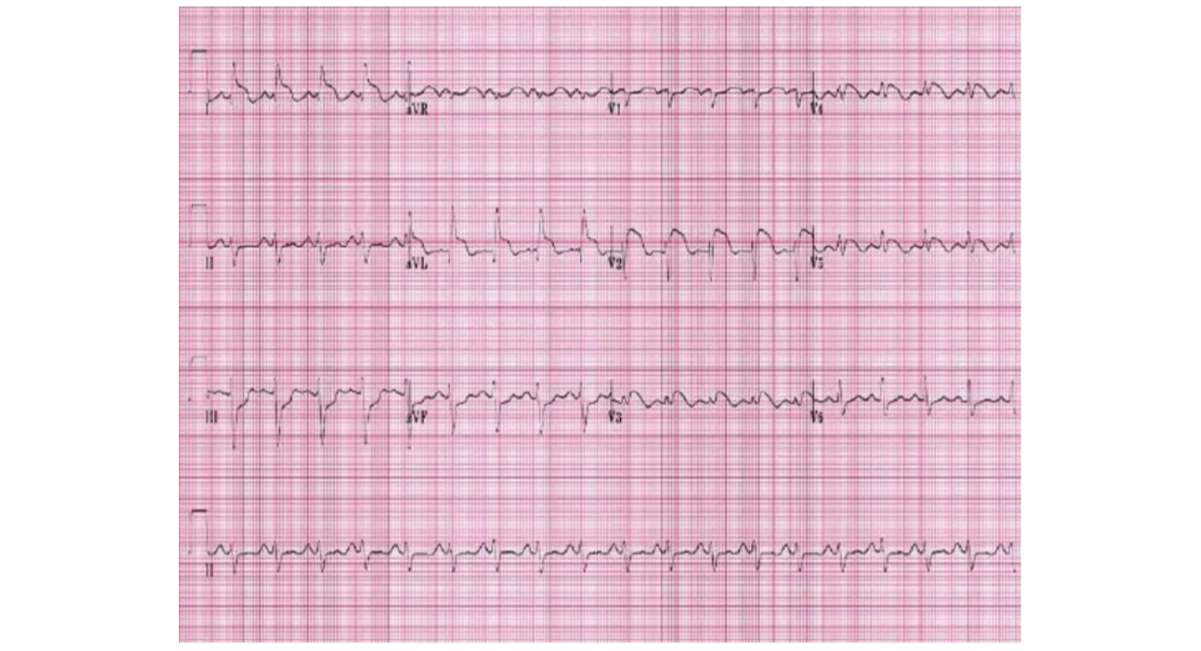
Figure 1: ECG showing acute anterior MI [4]
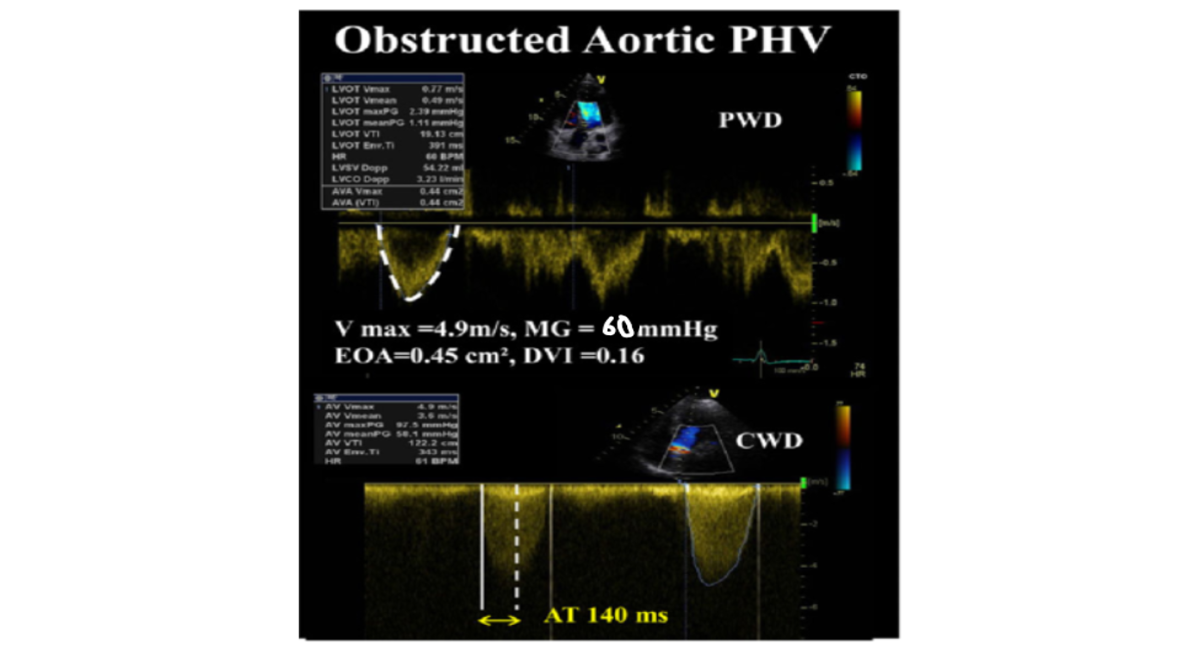
Figure 2: Echocardiogram readings, suggestive of severely stenosed prosthetic aortic valve [5]
NOTE: The patient presented at midnight, no time and storage were available to store his clinical images
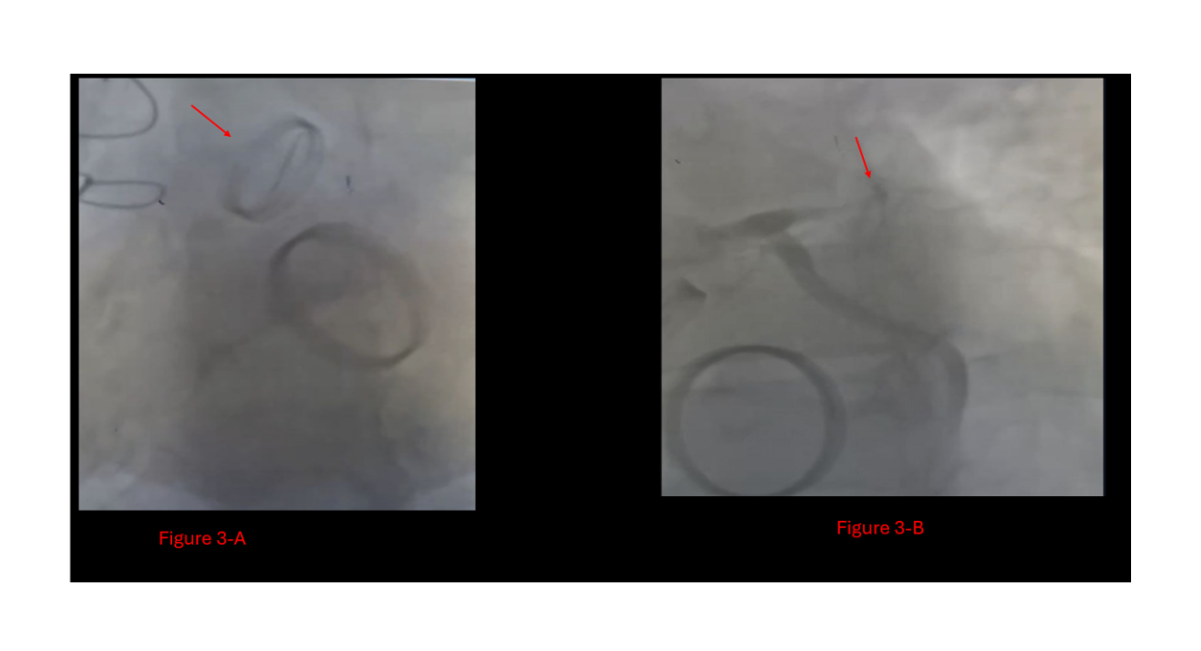
Figure 3: The fluoroscopy of the patient's admission,
A: Stuck prosthetic aortic valve with only one leaflet movement,
B: Total LAD occlusion by the proximal thrombus
Video 1: Patient's fluoroscopy at admission, showing the stuck aortic valve and the LAD thrombus
https://doi.org/10.5281/zenodo.17264772
Treatment
Although surgical valve replacement is the guideline-directed management for prosthetic valve thrombosis, the surgical team deemed the case too high-risk and declined intervention. Meanwhile, the previously pending INR was revealed to be 1.1 markedly subtherapeutic.
In this critical, life-threatening situation, the only viable management option was immediate thrombolytic therapy. A full dose of tenecteplase (Metalyse®) was administered one-fourth intracoronarily and the remaining three-fourths intravenously. The rationale was to address both the coronary occlusion and the prosthetic valve thrombosis in one attempt.
Following thrombolytic therapy, the patient's vital signs stabilized. Multiple runs of aspiration thrombectomy were performed. The patient’s hemodynamic status improved significantly, and he was transferred from the catheterization lab in stable condition, without stenting according to the deferred stent strategy (Figure 4).
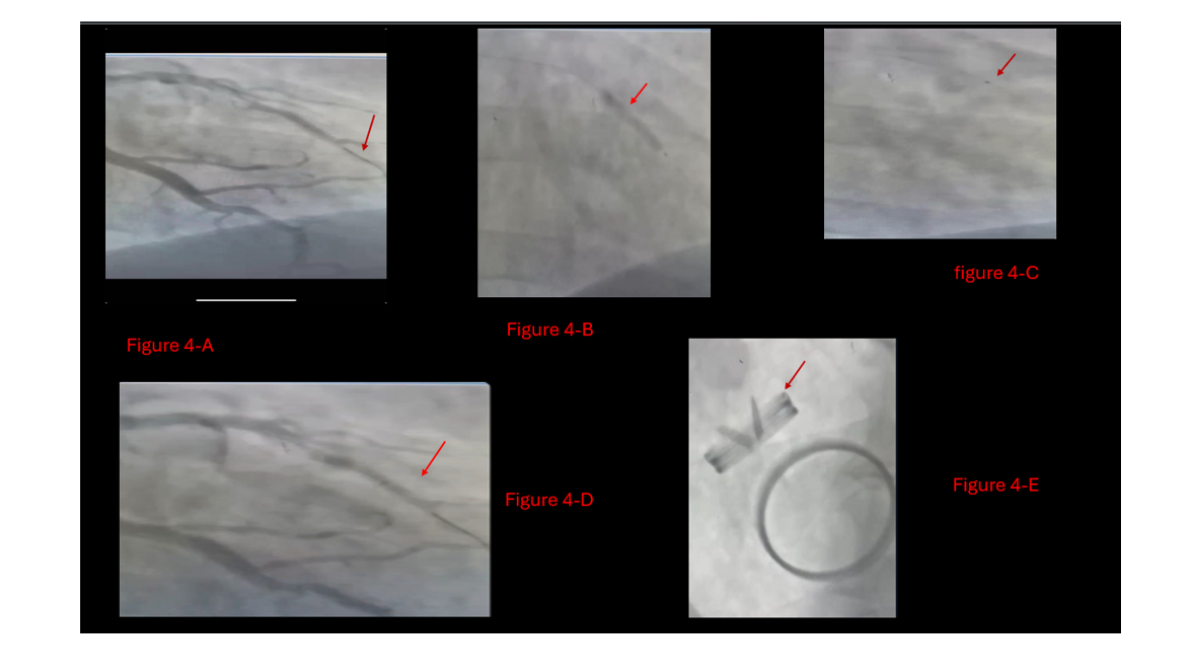
Figure 4: Patient`s LAD during catheterization,
A: Wire in LAD crosses the thrombotic lesion and after full dose of metalase,
B: LAD balloon dilation,
C: Aspiration catheterization,
D: After balloon dilation and multiple runs of aspiration catheterization, LAD is partially opened with TIMI flow II,
E: Aortic valve functioning well at the end of the intervention in the first day.
Outcome and Follow-up
The patient was admitted and started on therapeutic intravenous enoxaparin (Clexane®). On hospital day 3, a second-look coronary angiography showed partial thrombotic obstruction of the LAD, which was successfully treated with two further aspiration runs (Figure 5). Additionally, the aortic valve was now fully mobile with no evidence of residual thrombus (Video 2, Video 3). The patient was discharged on day 4 with a therapeutic INR, well-functioning aortic and mitral valves on echocardiogram, without any stent placement. His home medications included warfarin 5 mg daily and clopidogrel 75 mg daily.
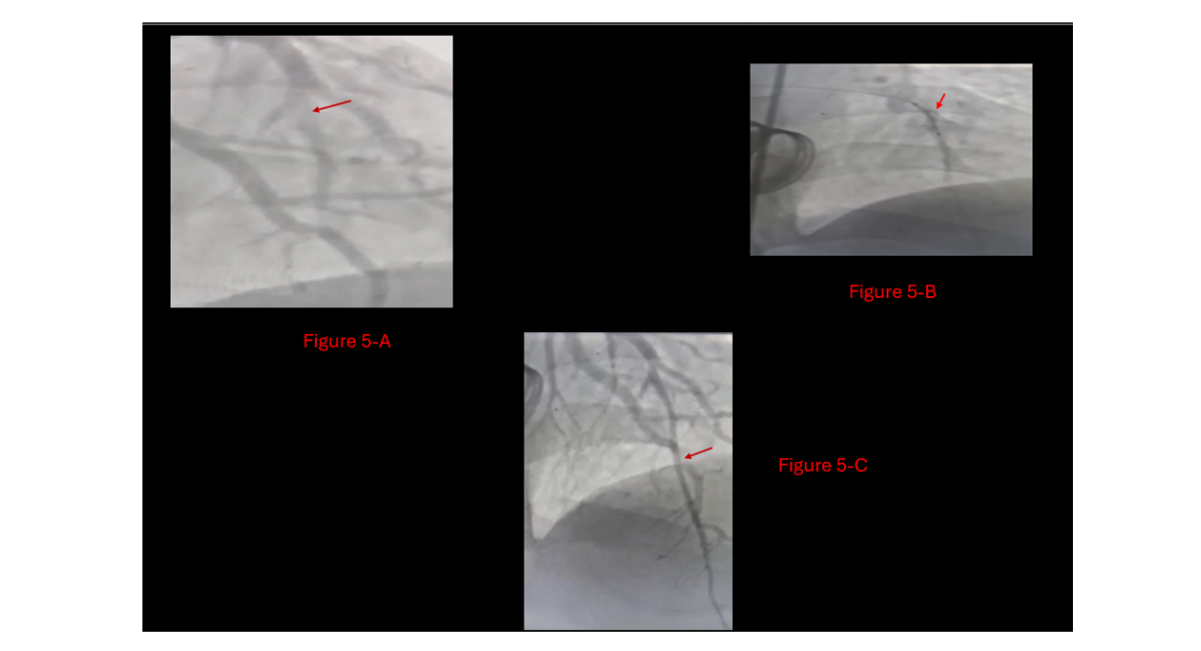
Figure 5: Last Catheter visit,
A: LAD showed residual thrombus at Diagonal 1,
B: second look with Balloon dilation at different levels of LAD,
C: Final result, patent LAD with TIMI flow III, without stenting need
Video 2: Totally patent LAD
https://doi.org/10.5281/zenodo.17264807
Video 3: Freely mobile prosthetic aortic valve
https://doi.org/10.5281/zenodo.17264821
DISCUSSION
This case illustrates the feasibility of off-label full-dose thrombolysis combined with aspiration thrombectomy in a critically ill patient with dual thrombotic pathology. This case supports the consideration of thrombolysis for high-risk patients, but more data is needed. This is a rare and highly complex case involving a 50-year-old male with a history of double mechanical valve replacement (aortic and mitral) on chronic warfarin therapy. The patient presented with symptoms of acute myocardial infarction (MI), which were ultimately attributed to coronary embolism arising from a stuck aortic valve a dual catastrophe.
The subtherapeutic INR of 1.1 raises concerns regarding inadequate follow-up, unadjusted anticoagulation doses, or possible patient non-compliance. These factors likely contributed to prosthetic valve thrombosis (PVT) and represent missed opportunities for prevention.
Multimodal imaging was crucial in this case. Transthoracic echocardiography revealed a high-pressure gradient across the aortic valve, indicative of obstruction. Fluoroscopy during coronary angiography identified both mechanical valve dysfunction and a coronary thrombus in the LAD, confirming the dual pathology.
Importantly, the radial approach to catheterization (rather than femoral) minimized bleeding risks a critical decision considering the need for systemic thrombolysis. If femoral access had been used, potential complications such as access-site bleeding or retroperitoneal hematoma could have compounded the patient’s critical status.
Another key decision was the recognition that the LAD obstruction was thrombotic, not a fixed atherosclerotic lesion. This avoided the common and unnecessary practice of stenting, which would not address the underlying pathology and might pose long-term harm.
The choice of full-dose thrombolytics (tenecteplase) administered one-quarter intracoronary and three-quarters intravenously was off-label but life-saving. This case underscores the importance of clinical flexibility and multidisciplinary decision-making, particularly when guideline-recommended surgical intervention is not feasible. With proper patient selection and careful administration, thrombolytic therapy can effectively treat both coronary and valvular thrombotic complications [6, 7].
The use of aspiration thrombectomy preserved the patient’s native coronary anatomy and avoided stenting. This approach is increasingly supported in literature as a suitable alternative for coronary embolism from valve thrombosis, when appropriate imaging and diagnosis are made.
Comparison to the Literature
According to our review, only two previously published cases closely resemble this presentation, though none were entirely typical [8, 9]. In our case, the use of full-dose tenecteplase (1/3 IC, 2/3 IV) diverges from the low-dose or ultraslow infusion regimens more commonly described in the literature. However, given the hemodynamic instability and coexisting MI, our approach was clinically appropriate and ultimately successful [10, 11].
Furthermore, the strategy of avoiding coronary stenting aligns with published cases of embolic MI from valve thrombus, where aspiration alone was sufficient to achieve full reperfusion [12].
Limitations
This single case limits broad conclusions, and more studies are needed to compare thrombolysis to surgery. The short follow-up period and the significant risks associated with thrombolysis, such as bleeding, need careful consideration in any future application of this approach.
Teaching Points
- Prevention is better than treatment: Long-term INR monitoring and patient education are essential in preventing mechanical valve thrombosis.
- Guidelines support but do not replace clinical judgment: When first-line surgical management is not feasible, thrombolysis is a reasonable and potentially life-saving second-line approach.
- Don’t treat the lesion—understand the mechanism: In coronary embolism, stenting is often unnecessary and avoidable.
- Multimodal imaging is essential: It allows early recognition of complex, multi-pathology presentations such as MI and prosthetic valve thrombosis.
CONCLUSION
Thrombolysis with aspiration was effective in this case, suggesting a potential option when surgery is not possible. This case contributes to the scarce literature on thrombolytic therapy in such dual presentations. This case represents a rare and highly complex clinical scenario that was resolved through a guideline-informed but clinically adapted approach. The patient presented with typical MI symptoms but had a history of double valve replacement, prompting early echocardiography and catheter-based imaging. Diagnosis of a stuck mechanical valve with embolic LAD thrombus was made via fluoroscopy and echocardiogram. Surgical management was not an option; therefore, a full therapeutic dose of thrombolytics, combined with multiple aspiration catheterizations, resulted in complete clinical recovery with no need for stenting or surgery. This case highlights that thrombolysis with aspiration was effective here, suggesting a potential option when surgery is not possible. This case highlights the importance of clinical reasoning, individualized therapy, and team-based decision-making in high-risk cardiovascular emergencies.
COMPETING INTERESTS
None
CONTRIBUTORSHIP
None
DISCLAIMER
The views expressed in the submitted article are the author's own and not an official opinion of the institution or funder.
FUNDING
No funding
ETHICAL APPROVAL
Ethical approval was obtained from the patient verbally
PATIENT AND PUBLIC INVOLVEMENT
No closed involvement
REFERENCES
- Deviri E, Sareli P, Wisenbaugh T, Cronje SL. Obstruction of mechanical heart valve prostheses: clinical aspects and surgical management. Journal of the American College of Cardiology. 1991;17(3):646-50. [Crossref] [Google Scholar] [PubMed]
- Mustapha R, Philip I, Bohm G, Depoix JP, Enguerand D, et. al. Thrombosis of heart valve prostheses: favourable and prognostic factors based on a study of 41 patients. In Annales de Chirurgie 1994 Vol. 48, No. 3, pp. 243-247. [Google Scholar] [PubMed]
- Roudaut R, Serri K, Lafitte S. Thrombosis of prosthetic heart valves: diagnosis and therapeutic considerations. Heart. 2007; 93(1):137-42. [Crossref] [Google Scholar] [PubMed]
- Guerra, W. (n.d.). Chest pain: EMS review [PowerPoint slides].
- Lancellotti P, Pibarot P, Chambers J, Edvardsen T, Delgado V, et, al. Recommendations for the imaging assessment of prosthetic heart valves: a report from the European Association of Cardiovascular Imaging endorsed by the Chinese Society of Echocardiography, the Inter-American Society of Echocardiography, and the Brazilian Department of Cardiovascular Imaging. European Heart Journal–Cardiovascular Imaging. 2016 ;17(6):589-90. [Crossref] [Google Scholar] [PubMed]
- Maxwell, Y. L. (2022, March 9). Thrombolysis ‘safe and effective’ for obstructive mechanical valve thrombosis. TCTMD.
- Bermejo J, Avanzas P. Comments on the 2021 ESC/EACTS guidelines for the management of valvular heart disease. Revista Espanola de Cardiologia. 2022;75(6):466-71. [Crossref] [Google Scholar] [PubMed]
- George JC, Buchanan D, Mazzoni J. Thrombectomy and fibrinolytic therapy of prosthetic valve thrombosis complicated by coronary embolism. The Journal of invasive cardiology. 2011; 23(1):E243-5. [Google Scholar] [PubMed]
- Nakazone MA, Tavares BG, Machado MN, Maia LN. Acute myocardial infarction due to coronary artery embolism in a patient with mechanical aortic valve prosthesis. Case reports in medicine. 2010; (1):751857. [Crossref] [Google Scholar] [PubMed]
- Al-Sarraf N, Al-Shammari F, Al-Fadhli J, Al-Shawaf E. Successful thrombolysis of a thrombosed prosthetic mitral valve using a synthetic tissue plasminogen activator: a case report. Journal of Medical Case Reports. 2010; 4(1):241. [Crossref] [Google Scholar] [PubMed]
- Serraino GF, Lorusso R, Renzulli A. Thrombolysis or operation: that is the question in prosthetic valve thrombosis. InFibrinolysis and Thrombolysis 2014. IntechOpen. [Crossref] [Google Scholar]
- Kavaliauskaite R, Otsuka T, Ueki Y, Räber L. Coronary embolism due to possible thrombosis of prosthetic aortic valve-the role of optical coherence tomography: case report. European Heart Journal-Case Reports. 2021;5(7):ytab115. [Crossref] [Google Scholar] [PubMed]
REFERENCES
Indexed In
DOAJ
CrossRef
PubMed
MEDLINE
ResearchBib
OAJI
Sindexs
EBSCO A-Z / Host
OCLC - WorldCat
Journal Flyer