ABSTRACT
Adverse drug effects are sometimes critical and fatal. Coronary artery and Zavras Kounis syndrome may not be the desired serious effects. Kounis Zavras (KZ) syndrome is an incidental occurrence of an acute coronary syndrome as a hypersensitivity reaction after exposure to an allergenic event. Salbutamol is a known β2-agonist commonly used as a bronchodilator therapy in the treatment of acute asthma. Oxygen is an important therapy in medicine. A mild COVID-19 infection means you have symptoms like cough, sore throat, and fatigue, but no dyspnea.
This report aims to describe a rare case of salbutamol-induced Kounis syndrome with sinus tachycardia in the setting of suspected mild COVID-19 pneumonia.
Keywords: Ephemeral Yasser's scooping ST-segment depression with giant T wave phenomenon; Oxygen; Salbutamol-induced Zavras Kounis syndrome; Mild COVID-19 pneumonia; Cardiovascular discovery and therapy.
INTRODUCTION
Bronchial asthma (BA) is an inflammatory and allergic lung disease. The prevalence of BA is a worldwide. Bronchoconstriction and wheeze are hallmarks of asthma [1]. Salbutamol is a selective B2-adrenoreceptor bronchodilator agonist used for the treatment and prevention of bronchial asthma and other reversible airways obstruction. Therefore, β-agonists have been prescribed as first-choice therapy for dramatic acute relief of asthma symptoms [2]. The common side effects are fine tremors, skipped heartbeats, anxiety, chest pain, headache, muscle cramps, and dry mouth. Arrhythmia, skin flushing, rare myocardial ischemia events, and disturbances of sleep and behavior may occur. There are rarely allergic reactions of paradoxical bronchospasms, hives, angioedema, hypotension, and collapse. Prolonged or high doses or use may cause hypokalemia [3]. Stevens-Johnson syndrome (SJS) and erythema multiforme can occur, especially in children, causing death [4]. Kounis Zavras (KZ) syndrome is defined as an incidental existence of an acute coronary syndrome (ACS) as a hypersensitivity reaction after an exposure to an allergenic event. It was originally described by Kounis and Zavras in 1991 and known as allergic angina syndrome [5]. According to the different studies, incidence rates of Kounis syndrome is reporting 19.4 per 100.000 among hospital admissions and 3.4% among allergy patients [6].
There is ACS-associated mast cell activation from allergic, hypersensitivity, or anaphylactoid reactions [7]. The essential pathogenesis of KS is the inflammatory cytokine mediators released through mast cell activation during a hypersensitivity reaction triggered by food, insect bites, or drugs. There is a subsequent coronary artery spasm (CAS) with possible atheromatous plaque erosion or rupture [7]. An allergic angina starts within one hour of exposure to the offending allergen. Longer onset of ACS has also been reported [8]. Variant presentations of KS have been reported [7]. Three different variants of KS have been described: Type I occurs in structurally normal coronary arteries with no cardiovascular risk factors. The coronary spasm was suggested with or without an associated acute myocardial infarction (AMI).
Type II KS occurs in patients with pre-existing ischemic heart disease (IHD), in whom the acute release of inflammatory mediators induces CAS that may lead to plaque rupture and MI. Type III KS occurs in patients with coronary artery stent-associated thrombosis [8-10]. Coronavirus disease 2019 (COVID-19) is a pandemic infectious disease caused by the severe acute respiratory syndrome coronavirus which has emerged globally since December 2019 from Wuhan, China [11]. Sometimes, included clinical associations, such as mild COVID-19 pneumonia, may be neglected and insignificant in data interpretation [12]. A mild COVID-19 infection means you have symptoms like cough, sore throat, and fatigue, but no dyspnea. Most patients who have mild COVID infections can be treated at home [13]. Most hospitalized patients of COVID-19 pneumonia show gradual functional recovery [14].
This manuscript reports a case of bronchial asthma complicated by salbutamol-induced Kounis syndrome with sinus tachycardia in a middle-aged female patient with suspected mild COVID-19 pneumonia.
CASE PRESENTATION
A 54-year-old, Nurse married female patient presented to the emergency department with an episode of bronchial asthma with chest pain and palpitation after inhalation of salbutamol. She was admitted to the intensive care unit (ICU) with Zavras Kounis syndrome with sinus tachycardia post-salbutamol inhalation in a suspected mild COVID-19 pneumonia. Ephemeral Yasser's scooping giant T-wave phenomenon and Zavras Kounis syndrome with sinus tachycardia post-salbutamol inhalation in a suspected mild COVID-19 pneumonia. Electrocardiography, chest CT, echocardiography, and oxygenation were the interventions. Clinical improvement and a dramatic reversal of the ECG changes had occurred.
Slight generalized body pains, fatigue, loss of appetite, and loss of smell were associated symptoms. The chest pain is angina. The patient had complained of a fever 5 days ago. She had direct contact with a confirmed case of COVID-19 pneumonia 10 days ago. The patient had a history of bronchial asthma 30 years ago. She appears distressed, irritable, and has tachypnea. Her vital signs were as follows: a regular heart rate of 100 bpm, blood pressure of 100/70 mmHg, respiratory rate of 25 bpm, a temperature of 36.3 °C, and a pulse oximeter of oxygen (O 2) saturation of 95%. GCS was 15. Generalized sibilant wheezes were heard on the chest auscultation. There are positive tests for latent tetany. No more relevant clinical data were noted during the clinical examination.
The patient was admitted to the intensive care unit (ICU) and was initially treated with O 2 inhalation by O 2 system line (100%, by standard mask, 5L/min; as needed). Paracetamol tablets (500mg, TDS as PRN) were added.
The initial ECG tracing on presentation in the ICU showed sinus tachycardia and ST-segment depression in I, II, V2, and V2–5 leads. There is a Wavy double sign (Yasser’s sign) of hypocalcemia in III lead, P-mitral, and epsilon waves (Figure 1A).
The second ECG tracing was done within 60 seconds of the above tracing and on the ICU admission showing sinus tachycardia, ST-segment depression in V2, and V3 leads, and marked ST-segment depression in a single beat with coincide giant T-wave in the same beat in V4–6 leads, followed by a Wavy triple sign (Yasser’s sign) in V4–5 leads, and Wavy double sign in V6 lead. There is also a Wavy double sign (Yasser’s sign) in aVR lead, a Wavy triple sign in I, and aVL leads. P-mitral, and epsilon waves (Figure 1B).
The third ECG tracing was taken within 20 seconds of the last tracing, during the ICU admission, and showed sinus tachycardia and ST-segment depression in I and V2–6 leads. There is a Wavy double sign in I lead and a Wavy triple sign in III lead. There is also a P-mitral and epsilon waves (Figure 1C).
The fourth ECG tracing was taken within 8 hours of the above tracings, and after oxygen inhalation, showing a normal sinus rhythm with normalization of all the above abnormalities. There are still epsilon waves (Figure 1D).
The initial complete blood count (CBC); Hb was 12.3 g/dl, RBCs; 4.4610³/mm³, WBCs; 5.910³/mm³ (Neutrophils; 90.3 %, Lymphocytes: 7.6%, Monocytes; 2.1%, Eosinophils; 0% and Basophils 0%), HCT was 37.7%, and Platelets; 137*10³/mm³. D-dimer was (0.44 ng/ml). INR was 1.04. PT was 13 seconds. CRP was negative. The troponin test was negative. SGPT was (45 U/L) and SGOT was (76 U/L). Serum albumen was normal (4.1 gm/dl). Serum creatinine was (1.4 mg/dl). RBS was (96 mg/dl). HBsAg was negative. HCA was negative. HIVab was negative. Serum potassium was (3.8 mmol/L). Plasma sodium was (143 mmol/L). Serum ionized calcium was (0.9 mmol/L).
Immediate ABG was (PH; 7.48, PCO2; 30 mmHg, HCO3; 24 mmHg, SO2; 94%, and PaO2; 81 mmHg).
The initial chest CT scan on presentation showed left reversed halo sign with small ground-glass opacity (Figure 2A). The plain film of the initial chest CT scan on presentation showed left Para-hilar crescent-like ground-glass opacity (Figure 2B). The plain CXR, PA view film of presentation showed left Para-hilar crescent-like opacity (Figure 2C).
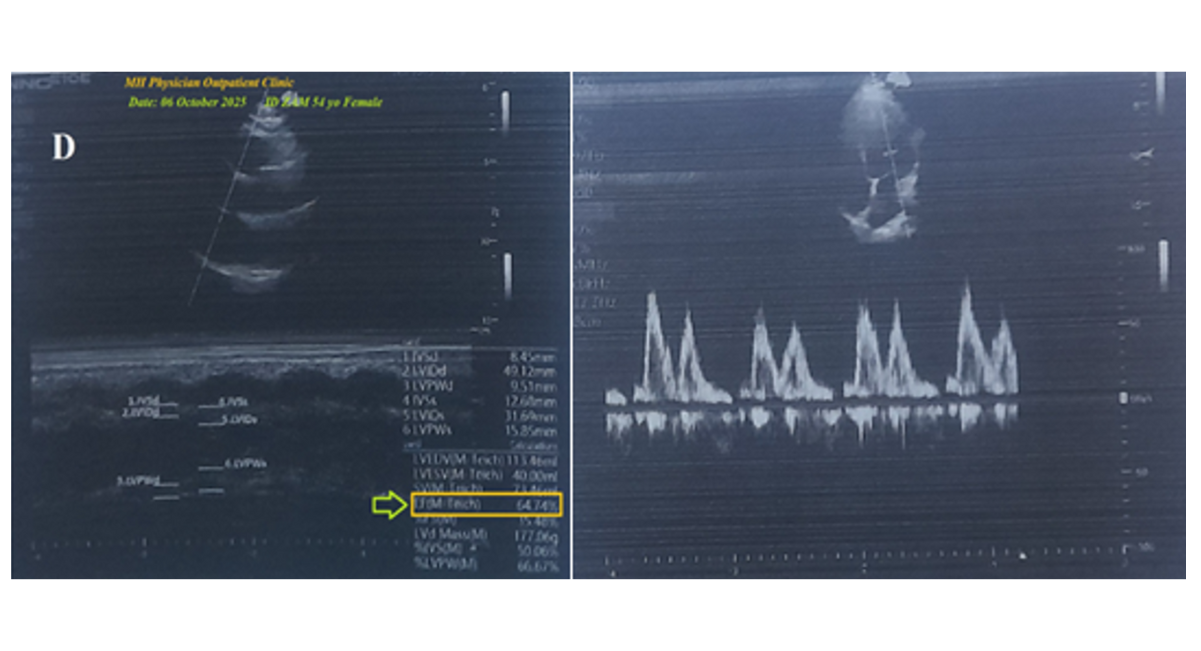
The echocardiography showed no abnormalities detected with a normal ejection fraction (EF: 64.74%) (Figure 2D). There is no more workup and radiological imaging.
Ephemeral Yasser's scooping giant T wave phenomenon in oxygen relieving salbutamol-induced Zavras-Kounis syndrome in a suspected mild COVID-19 pneumonia was the most probable provisional diagnosis.
Within 12 hours of management, a dramatic clinical and ECG improvement had occurred. Within 24 hours post-stabilization, she was discharged and continued on calcium and vitamin D preparation tablets for 2 weeks with advised cardiac and chest follow-up.
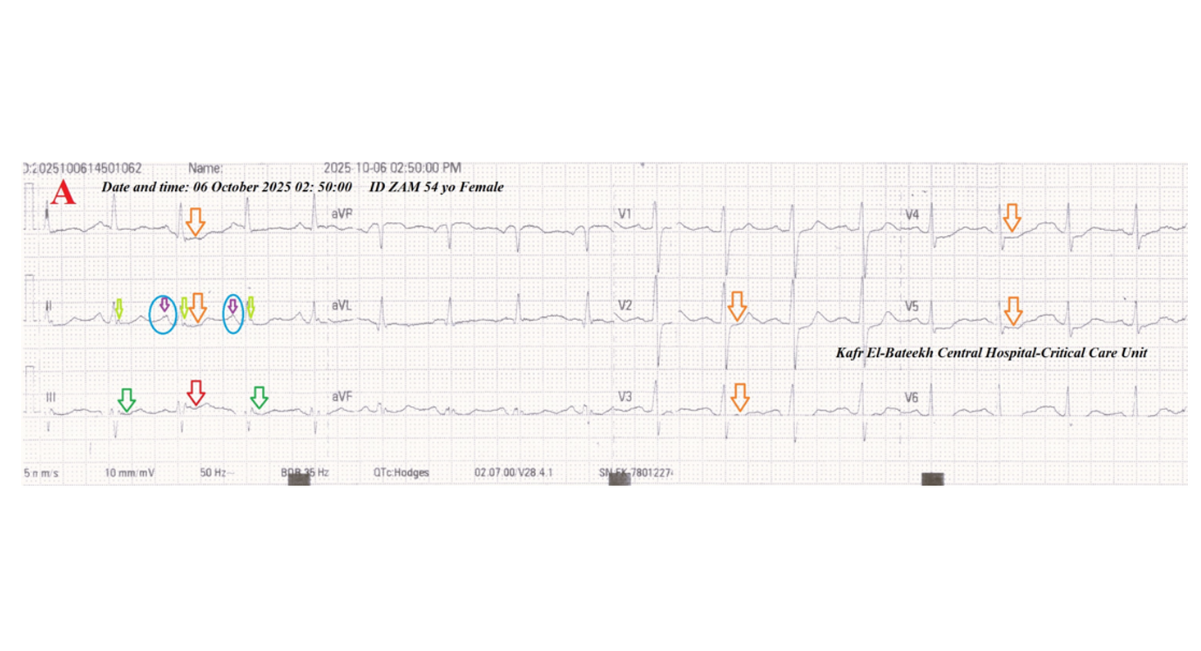
Figure 1A: Serial ECG tracings were done. ECG tracing was done on the presentation in the ICU, showing sinus tachycardia (VR; 101) and ST-segment depression in I, II, V2, and V2-5 leads (golden arrows). There is a Wavy double sign of hypocalcemia in III lead (green and red arrows), P-mitral (light blue circles and purple arrows), and epsilon waves (lime arrows).
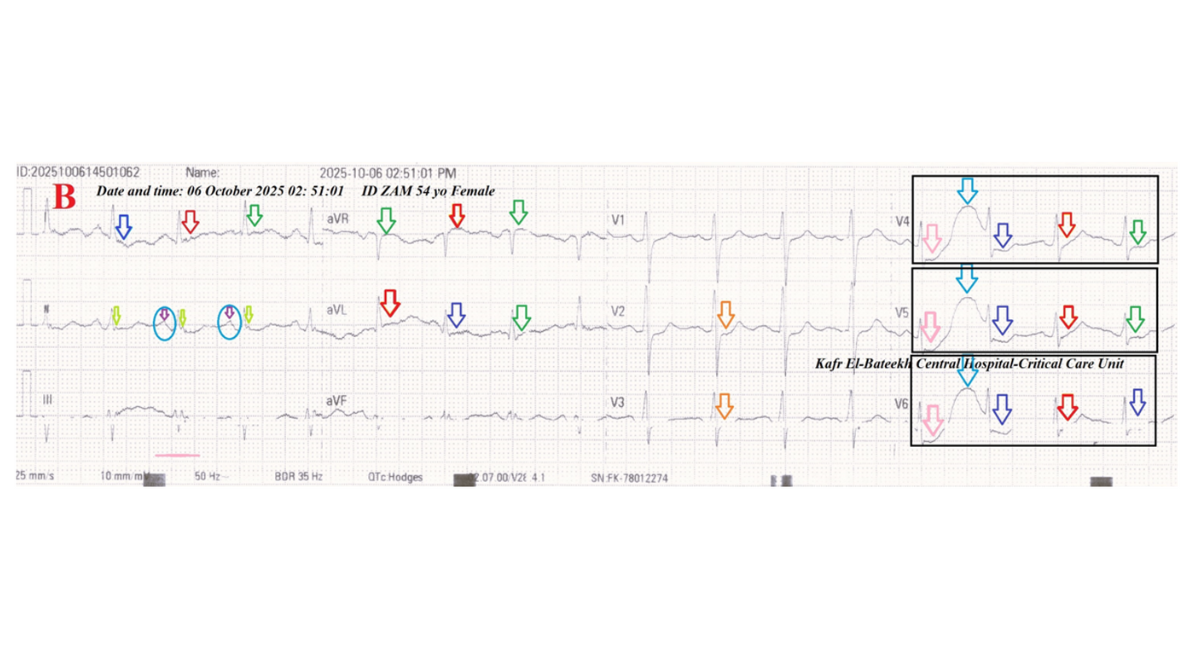
Figure 1B: ECG tracing was done within 60 seconds of the above tracing and on the ICU admission showing sinus tachycardia (VR;100) and sinus tachycardia (VR; 100), ST-segment depression in V2, and V3 leads (golden arrows), and marked ST-segment depression in a single beat (rose arrows) with coincide giant T-wave in the same beat (light blue arrows) in V4-6 leads, followed by a Wavy triple sign in V4-5 leads (dark blue, green, and red arrows), and Wavy double sign in V6 lead (dark blue and red arrows). There is also a Wavy double sign in aVR lead (green and red arrows), a Wavy triple sign in I and aVL leads (dark blue, green, and red arrows). P-mitral (light blue circles and purple arrows), and epsilon waves (lime arrows).
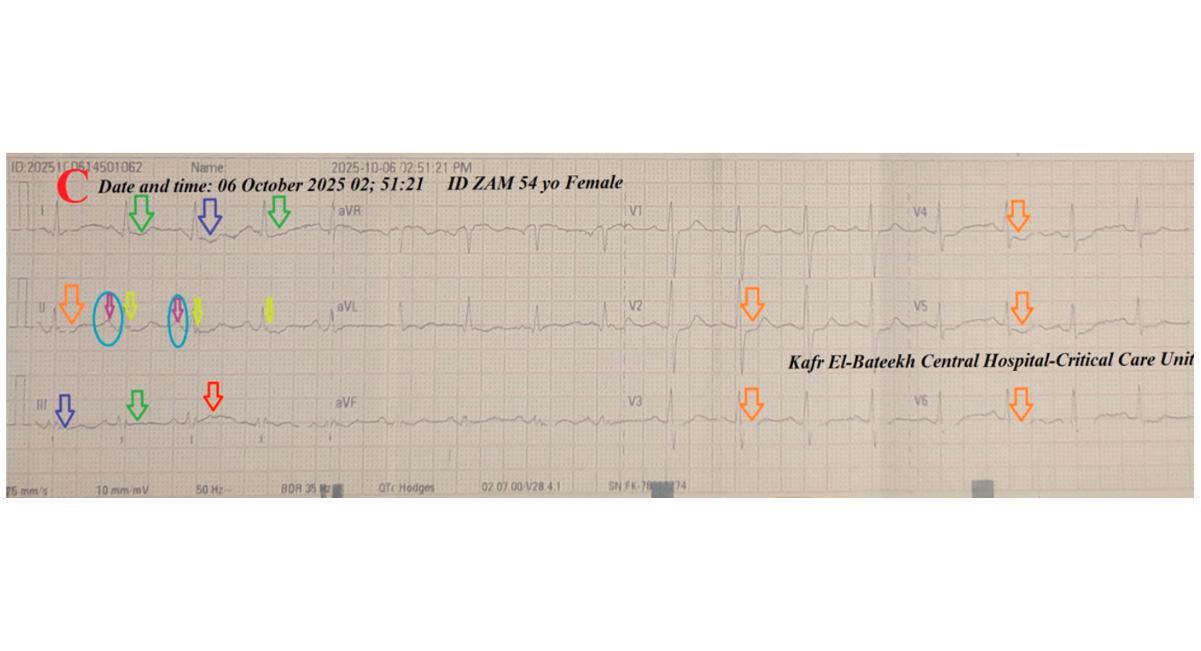
Figure 1C: ECG tracing done within 20 seconds of the last tracing, on the ICU admission, showing sinus tachycardia (VR; 102) and ST-segment depression in I and V2-6 leads (golden arrows). There are Wavy double sign in I lead (dark blue and green arrows) and Wavy triple sign in III lead (dark blue, green, and red arrows). There is also a P-mitral (light blue circles and purple arrows) and epsilon waves (lime arrows).
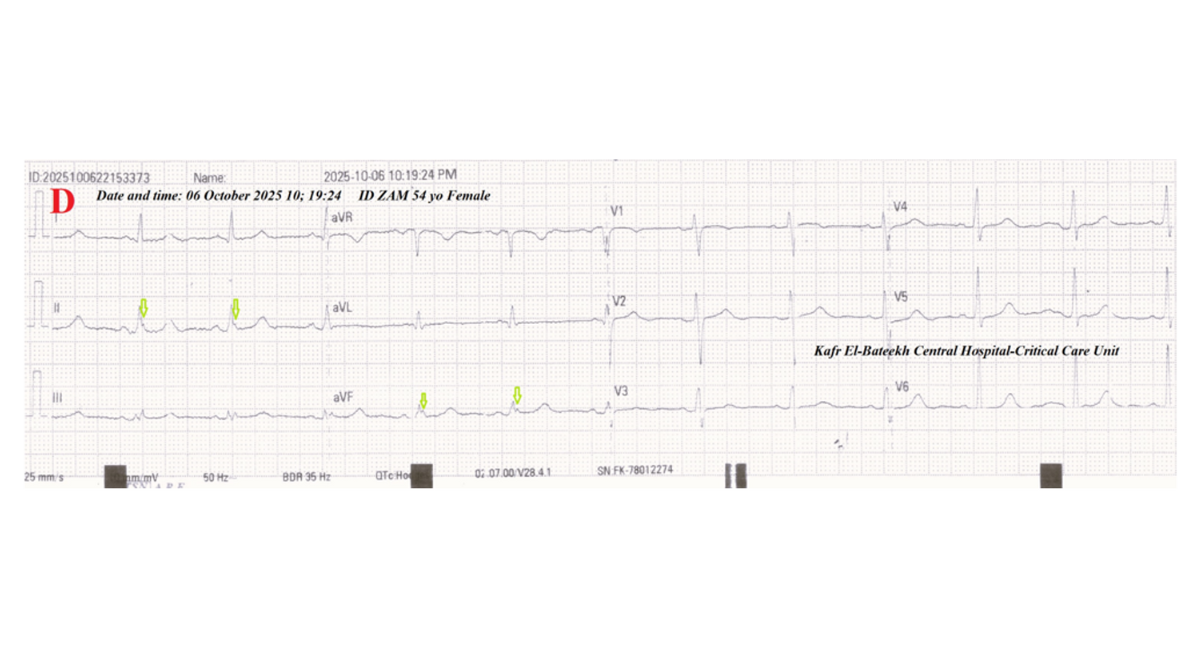
Figure 1D: ECG tracing was done within 8 hours of the above tracings and after oxygen inhalation, showing a normal sinus rhythm (VR; 72) with normalization of all the above abnormalities. There are still epsilon waves (lime arrows).
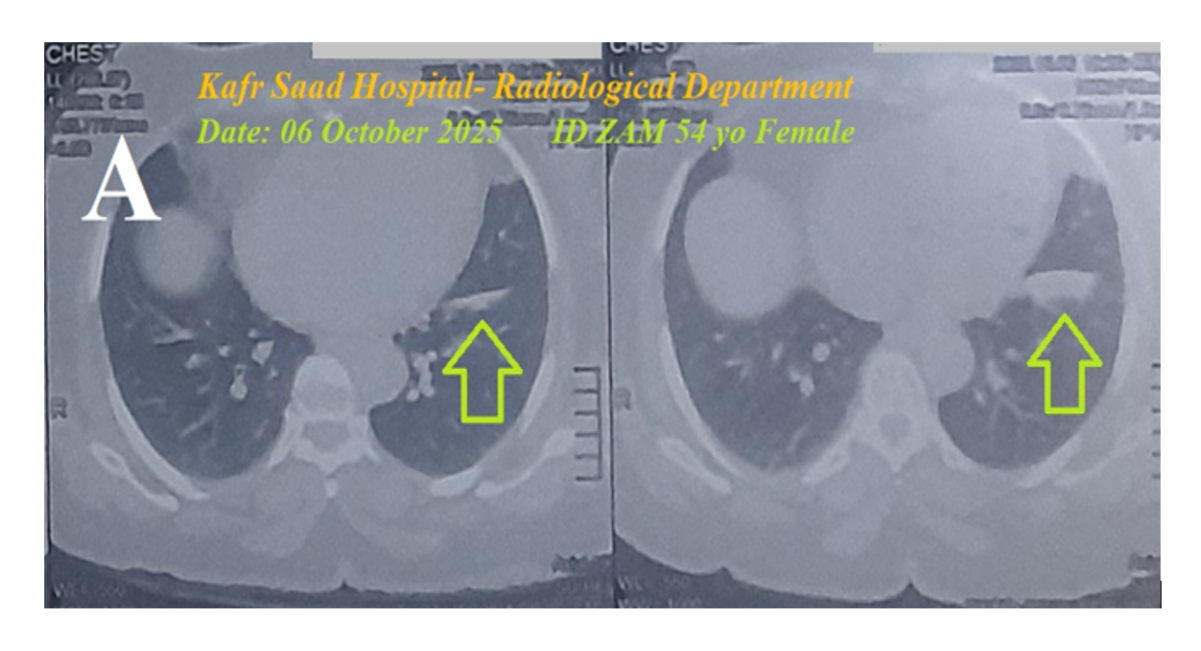
Figure 2A: The initial chest CT scan on presentation showed left reversed halo sign with small ground-glass opacity (lime arrows).
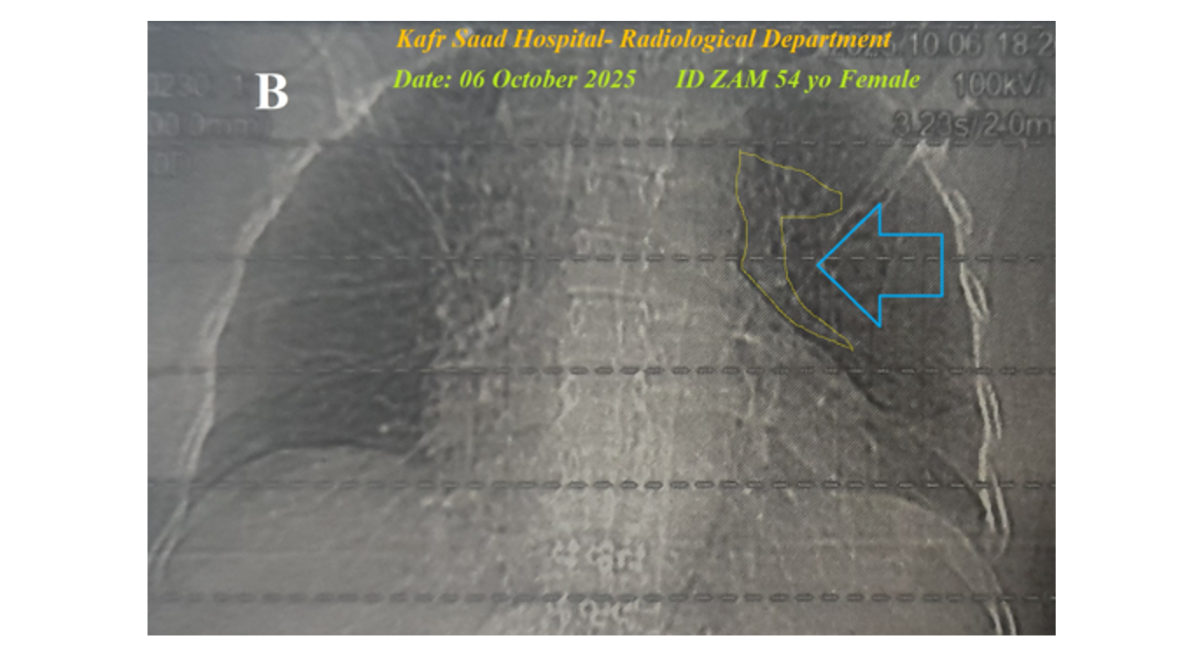
Figure 2B: The plain film of the initial chest CT scan on presentation showed left Para-hilar crescent-like ground-glass opacity (Yasser's lateral halo sign; yellow lining and light blue arrow).
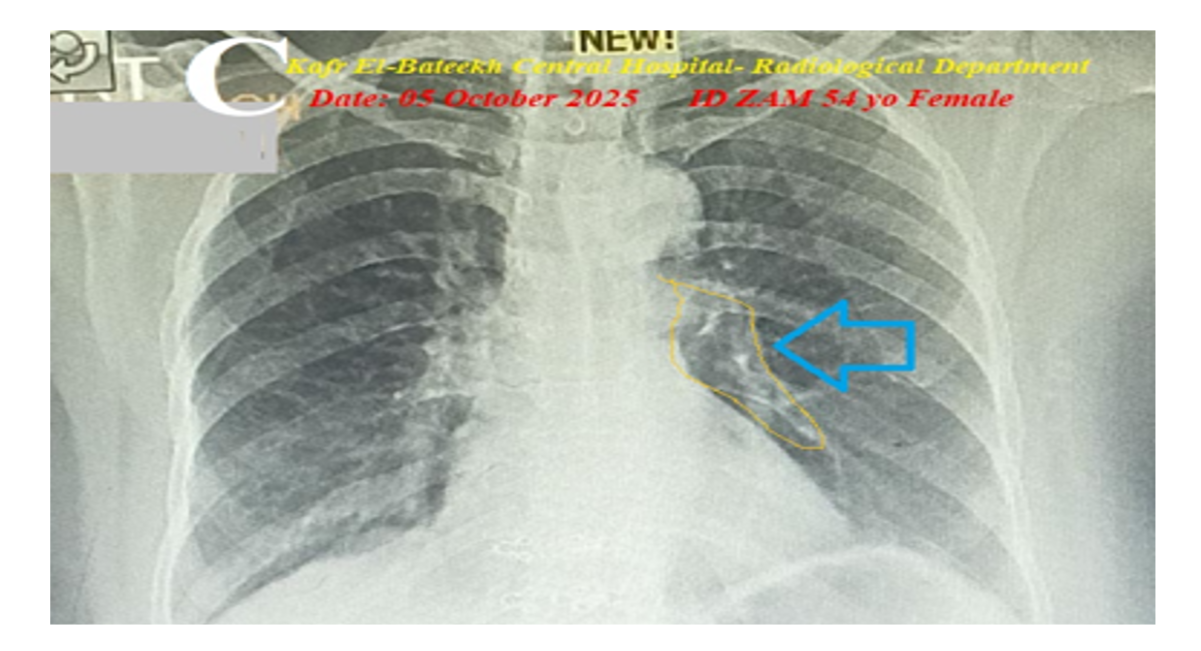
Figure 2C: The plain CXR, PA view film of presentation showed left Para-hilar crescent-like opacity (Yasser's lateral halo sign; yellow lining and light blue arrow).
DISCUSSION
An episode of bronchial asthma, admitted to the ICU with Zavras-Kounis syndrome with sinus tachycardia post-salbutamol inhalation in a suspected mild COVID-19 pneumonia in a middle-aged female patient. The primary objective for this case study was the presence of a patient with Zavras-Kounis syndrome with sinus tachycardia post-salbutamol inhalation in a suspected mild COVID-19 pneumonia in a middle-aged female patient in the ICU. The secondary objective for this case study was the question of how to manage the case in the ICU. A positive history of contact with a confirmed COVID-19 case, reversal halo sign, Yasser's lateral halo sign with small left ground-glass consolidation, and CBC evidence of COVID-19 suspicion on top of clinical COVID-19 presentation with slight generalized body pains, fatigue, loss of appetite, and loss of smell will strengthen the higher suspicion of mild COVID-19 diagnosis. The presence of angina chest pain, palpitation, and ECG evidence of ST-segment depression (Figures 1A, 1B, and 1C) after inhalation of salbutamol suggested that salbutamol is an implicated cause. After exclusion of other possible triggers in the current case, Naranjo's probability scale was used to evaluate the association between salbutamol inhalation and the associated symptoms [15]. Naranjo's probability scale in the current case study was +11. This means that there was a definite relationship between these adverse drug reactions and salbutamol inhalation (Table 1).
The reversal of ECG ST-segment depression after oxygen inhalation will strengthen its role in the management of ischemic heart disease. Coronary artery spasm is the interpretative mechanism in the reversal of ECG ST-segment depression. There is a deep scooping of ST-segment depression with a coincident giant T wave in a single beat in a serial manner of V4-6 leads (Figure 1B). Both deep scooping of ST-segment depression with a coincident giant T wave in a single beat of the same lead are followed by a Wavy triple sign in V4-5 leads and a Wavy double sign in V6 lead, and sinus tachycardia (Figure 1B). The four components: A. deep scooping of ST-segment depression, B. a coincident giant T wave in a single beat, C. sinus tachycardia, and D. both associated Wavy triple sign and Wavy double sign, an accidental association of unknown previously described. These three components disappear spontaneously or after oxygen inhalation. The appearance and disappearance of these four components are newly described as "Ephemeral Yasser's scooping ST-segment depression with giant T wave phenomenon" (Figure 3). The phenomenon is composed of passing sinus tachycardia, ST-segment depression in V2 and V3 leads, and marked ST-segment depression in a single beat with a coincident giant T-wave in the same beats in V4-6 leads, followed by a Wavy triple sign in V4-5 leads, and a Wavy double sign in V6 lead (Figure 1B).
There are no known mechanisms explaining this new phenomenon. The sector transient coronary artery spasm with associated hypocalcemia may be a suggestive theory for interpretation. Tachypnea may be the cause of associated acute respiratory alkalosis and subsequent hypocalcemia. I can’t compare the current case with similar conditions. There are no similar or known cases with the same management for near comparison. The Tee Pee sign and acute ST-segment elevation myocardial infarction may be included in the differential diagnosis. But the ECG criteria are against them. The only limitation of the current case study was the coronary angiography.
|
Question |
Yes |
No |
Do Not Know |
Score |
|
Are there previous conclusive reports on this reaction? |
1 |
0 |
0 |
1 |
|
Did the adverse event appear after the suspected drug was administered? |
2 |
-1 |
0 |
2 |
|
Did the adverse event improve when the drug was discontinued or a specific antagonist was administered? |
1 |
0 |
0 |
1 |
|
Did the adverse event reappear when the drug was re-administered? |
2 |
-1 |
0 |
2 |
|
Are there alternative causes that could on their own have caused the reaction? |
-1 |
2 |
0 |
2 |
|
Did the reaction reappear when a placebo was given? |
-1 |
1 |
0 |
0 |
|
Was the drug detected in blood or other fluids in concentrations known to be toxic? |
1 |
0 |
0 |
0 |
|
Was the reaction more severe when the dose was increased or less severe when the dose was decreased? |
1 |
0 |
0 |
1 |
|
Did the patient have a similar reaction to the same or similar drugs in any previous exposure? |
1 |
0 |
0 |
1 |
Table 1: Naranjo Algorithm-Adverse Drug Reaction (ADR) Probability Scale in the case report.
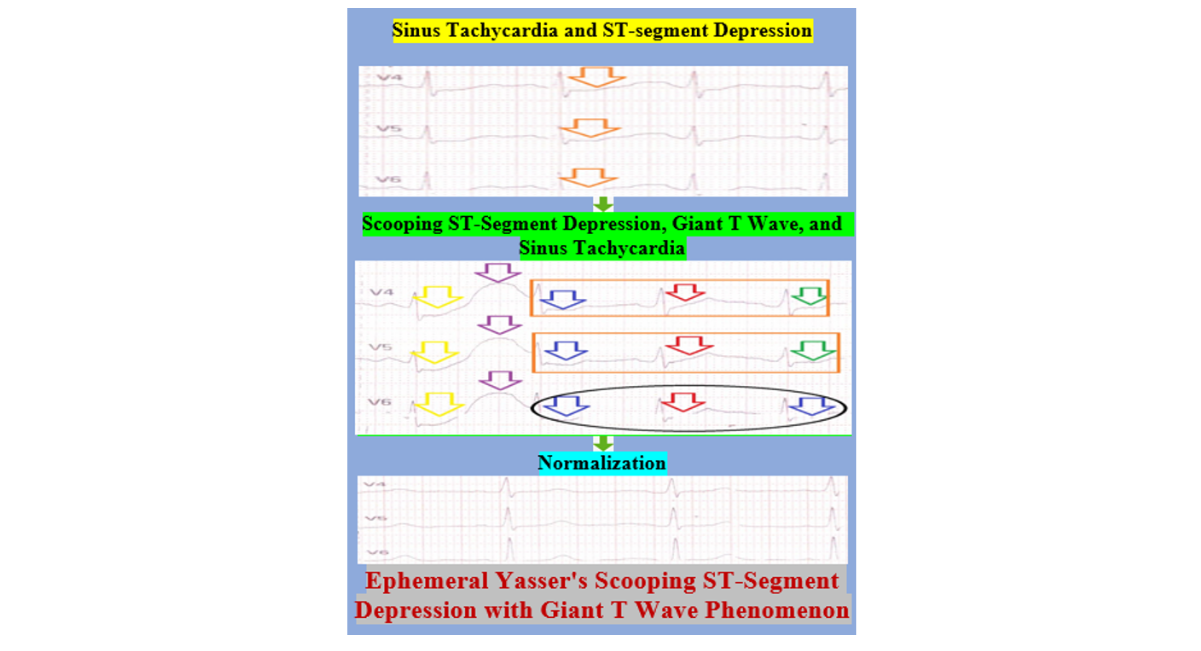
Figure 3: Graphical abstract of Ephemeral Yasser's scooping ST-segment depression with giant T wave phenomenon
CONCLUSION AND RECOMMENDATIONS
Ephemeral Yasser's scooping ST-segment depression with giant T-wave phenomenon is a newly described transitory cardiovascular phenomenon. It has four components: A. deep scooping of ST-segment depression, B. a coincident giant T wave in a single beat, C. sinus tachycardia, and D. both associated Wavy triple sign (Yasser’s sign) and Wavy double sign (Yasser’s sign). Oxygen responded to salbutamol, inducing Kounis Zavras (KZ) syndrome, signifying the reversal role of oxygen in coronary artery spasm. The initial priority of management for cardiologists, intensivists, and emergency physicians should be directed to eliciting the probable drug's adverse effects.
CONFLICTS OF INTEREST
There are no conflicts of interest.
ACKNOWLEDGMENT
The author wish to thank:
The team of critical care nurses at Kafr El-Bateekh Central Hospital for their assistance data entry and extra ECG copies. Also, he would like to thank his partner for their unwavering support and patience throughout this research.
ABBREVIATIONS
CAS: Coronary artery spasm
ECG: Electrocardiogram
ED: Emergency department
ICU: Intensive care unit
KS: Zavras Kounis syndrome
MI: Myocardial infarction
O2: Oxygen
VR: Ventricular rate
REFERENCES
- Marques L, Vale N. Salbutamol in the management of asthma: A review. International Journal of Molecular Sciences. 2022 ;23(22):14207. [Crossref] [Google Scholar] [PubMed]
- Martin MJ, Harrison TW. Is it time to move away from short-acting beta-agonists in asthma management? Eur Respir J. 2019;53(4). [Crossref] [Google Scholar] [PubMed]
- British National Formulary. Selective beta2 agonists – side effects. 57 edition. London: BMJ Publishing Group Ltd and Royal Pharmaceutical Society Publishing. 2008. ISBN 978-0-85369-778-7.
- Ishver A. Albuterol (Proventil, Ventolin, and others) - Uses, Side Effects, and More.
- Fassio F, Losappio L, Antolin-Amerigo D, Peveri S, Pala G, et, al. Kounis syndrome: a concise review with focus on management. Eur J Intern Med. 2016;30:7-10. [Crossref] [Google Scholar] [PubMed]
- Forzese E, Pitrone C, Cianci V, Sapienza D, Ieni A, et al. An insight into Kounis syndrome: bridging clinical knowledge with forensic perspectives. Life. 2024;14(1):91. [Crossref] [Google Scholar] [PubMed]
- Memon S, Chhabra L, Masrur S, Parker MW. Allergic acute coronary syndrome (Kounis syndrome). Proc (Bayl Univ Med Cent). 2015 ;28(3), pp. 358-362). Taylor & Francis. [Crossref] [Google Scholar] [PubMed]
- Abdelghany M, Subedi R, Shah S, Kozman H. Kounis syndrome: a review article on epidemiology, diagnostic findings, management and complications of allergic acute coronary syndrome. International Journal of Cardiology. 2017;232:1-4. [Crossref] [Google Scholar] [PubMed]
- Kounis NG. Kounis syndrome: an update on epidemiology, pathogenesis, diagnosis and therapeutic management. Clin Chem Lab Med. 2016;54(10):1545-59. [Crossref] [Google Scholar] [PubMed]
- Hermans MA, Roeters van Lennep JE, Van Daele PL, Bot I. Mast cells in cardiovascular disease: from bench to bedside. Int J Mol Sci. 2019;20(14):3395. [Crossref] [Google Scholar] [PubMed]
- Islam MA, Kundu S, Alam SS, Hossan T, Kamal MA, et al. Prevalence and characteristics of fever in adult and paediatric patients with coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis of 17515 patients. PloS one. 2021;16(4):e0249788. [Crossref] [Google Scholar] [PubMed]
- Elsayed YM. False Angina and Mimic Myocardial Infarction in Wavy Triple Sign (Yasser’s Sign) of Hypocalcemia with later mild COVID-19 Pneumonia-Differentiation and Outcome. J Cri Res & Eme Med, 2 (1), 01. 2023;4. [Crossref] [Google Scholar] [PubMed]
- Armitage M. What Are the Mild Symptoms of COVID, and When Should You See a Doctor? 2024
- Cha MJ, Solomon JJ, Lee JE, Choi H, Chae KJ, et al. Chronic lung injury after COVID-19 pneumonia: clinical, radiologic, and histopathologic perspectives. Radiology. 2024;310(1):e231643. [Crossref] [Google Scholar] [PubMed]
- Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239-45. [Crossref] [Google Scholar] [PubMed]
Article Processing Timeline
| 2-5 Days | Initial Quality & Plagiarism Check |
| 15 Days |
Peer Review Feedback |
| 85% | Acceptance Rate (after peer review) |
| 30-45 Days | Total article processing time |
Indexed In
ResearchBib
Sindexs
OAJI
DOAJ
CrossRef
PubMed
MEDLINE
EBSCO A-Z / Host
OCLC - WorldCat
Journal Flyer